Every day, healthcare administrators make decisions that ripple through their organizations, directly impacting patient safety and clinical outcomes. While the principle of non-maleficence (“first, do no harm”) is a bedrock of clinical practice, its true defense is built long before a patient ever enters a room. It is forged in budget meetings, staffing models, and vendor contracts.
In an era of persistent workforce shortages and financial pressure, the link between strategic staffing and ethical patient care has never been more critical. Can we truly say we are avoiding harm if our staffing strategies are reactive, fragmented, or limited to a narrow pool of resources?
This article explores the profound responsibility healthcare leaders carry in operationalizing non-maleficence. We will examine how proactive, ethically-minded staffing is a moral imperative, and how embracing a more democratic approach to talent acquisition can build a more resilient, safe, and equitable future for your organization and the patients you serve.
What Is Non-Maleficence?
Derived from the Latin phrase primum non nocere, or “first, do no harm,” it is one of the core tenets of biomedical ethics. In essence, non-maleficence is the ethical charge to remove or mitigate risks within the healthcare environment. It is the directive that should guide decisions on resource allocation, staffing models, technology implementation, and quality improvement initiatives. Beyond the absence of malicious intent, non-maleficence requires the presence of vigilant, system-wide safeguards.
For the healthcare administrator, non-maleficence is an organizational mandate. It means creating and maintaining systems, policies, and a culture that proactively prevent harm to patients, staff, and the community. This encompasses:
- Clinical Harm: This is the most direct interpretation, including preventable medical errors, hospital-acquired infections, and unsafe medication practices.
- Psychological and Emotional Harm: This involves protecting patients from disrespect, dismissive communication, or trauma resulting from their care experience.
- Systemic Harm: This is the administrator’s primary domain. It refers to harm caused by organizational failures such as understaffing, poorly designed workflows, inadequate equipment, or a culture that leads to burnout and reduced quality of care.
Why Is Non-Maleficence Important?
Healthcare is a profession built on a covenant of trust. Patients and families enter our facilities at their most vulnerable, trusting that the system will help, not hurt them. Upholding non-maleficence is fundamental to maintaining this sacred trust. Breaches of this trust, through preventable harm, erode the very foundation of the patient-provider relationship and damage the institution’s integrity.
Furthermore, a culture focused on preventing harm is intrinsically linked to reliable performance. Systems designed with non-maleficence as a priority are inherently safer, more efficient, and produce better outcomes. It’s important to keep in mind that the financial ramifications of a single adverse event can be staggering. Investing in systems that prevent harm (such as safe staffing, robust training, and predictive analytics) also protects the organization’s bottom line.
What Role Does Healthcare Staffing Have in Protecting Non-Maleficence?
Staffing decisions are one primary mechanism through which an organization fulfills its duty to avoid harm. From an administrative lens, staffing is the strategic variable that either reinforces or erodes a culture of safety. A robust staffing model protects non-maleficence by serving as the first line of defense against a cascade of potential harms. Conversely, chronic understaffing creates a high-risk environment where errors are not a matter of if, but when. The relationship is direct and causal, impacting safety in several key areas.
5 Ways Proactive Healthcare Staffing Protects Patients
Moving from a reactive model of “filling shifts” to a proactive strategy of “building safe teams” is one of the most powerful actions an administration can take. Proactive staffing uses data, forecasting, and strategic planning to ensure the right number and mix of staff to operationalize the ethical duty of non-maleficence. Here are five key ways it protects patients:
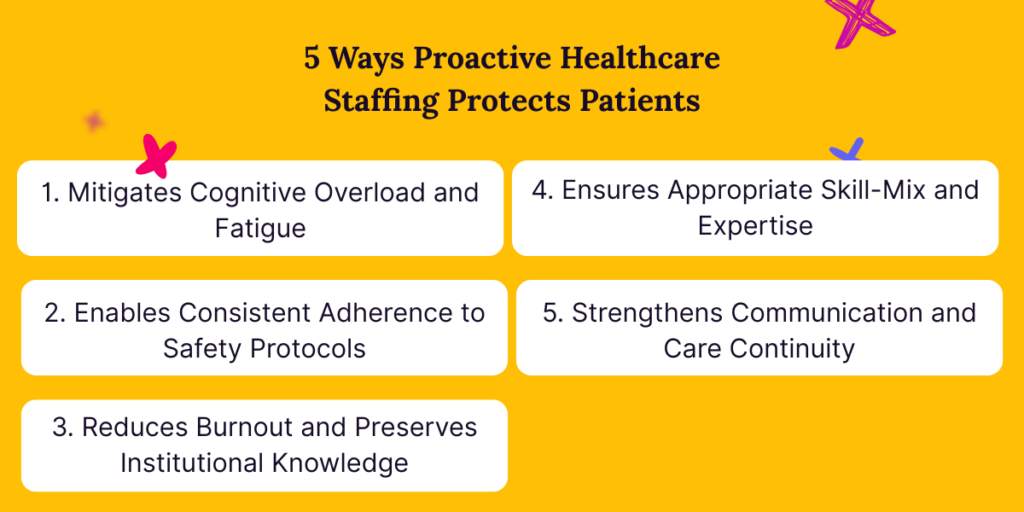
1. Mitigates Cognitive Overload and Fatigue
Proactive staffing ensures workloads are manageable, preserving clinicians’ critical cognitive bandwidth. When physicians are not stretched beyond their capacity, they maintain the vigilance needed to catch subtle changes in a patient’s condition, double-check medication orders, and adhere to complex safety protocols. This directly reduces diagnostic errors, medication mistakes, and failure-to-rescue events.
2. Enables Consistent Adherence to Safety Protocols
From central line bundles and VAP prevention to fall risk assessments, safety protocols require time and attention. An understaffed unit forces corners to be cut. Proactive staffing provides the necessary time and resources for clinicians to consistently and meticulously follow every step of evidence-based practices, creating a reliable defense against hospital-acquired conditions.
3. Reduces Burnout and Preserves Institutional Knowledge
Chronic short-staffing is a primary driver of clinician burnout and turnover. A proactive approach demonstrates an organizational commitment to staff well-being, which improves retention. This stability preserves invaluable institutional knowledge and fosters experienced, cohesive teams who understand unit-specific workflows and patient populations, leading to safer, more efficient care.
4. Ensures Appropriate Skill-Mix and Expertise
Proactive staffing goes beyond mere numbers; it ensures the right skills are in the right place at the right time. By analyzing patient acuity data and forecasting needs, administrators can strategically deploy specialized expertise (e.g., critical care, oncology) and maintain a balanced skill-mix on each shift. This prevents scenarios where less-experienced staff are placed in situations beyond their competency, a known risk factor for patient harm.
5. Strengthens Communication and Care Continuity
A stable, well-staffed environment fosters better communication. With manageable patient assignments, clinicians have the time for thorough handoffs, interdisciplinary rounds, and meaningful conversations with patients and families. Furthermore, reducing reliance on temporary staff minimizes care fragmentation, ensuring that the team caring for a patient has a deep, continuous understanding of their history and plan, which is critical for preventing errors.
Non-Maleficence and the Democratization of Healthcare Staffing
The principle of non-maleficence compels us to look beyond the bedside and examine the systems that enable safe care. This includes the very marketplace from which we source vital temporary clinical staff. A consolidated, limited staffing industry can, perhaps unintentionally, create systemic harm by restricting choice, inflating costs, and making it difficult for organizations, especially smaller or rural ones, to access the quality talent they need to protect their patients.
True adherence to non-maleficence in staffing requires a market that is robust, competitive, and equitable. This is the core of democratization: breaking down barriers to entry and creating a fair playing field. By actively partnering with a diverse network of small, women-owned, and minority-owned locum tenens agencies, healthcare administrators can directly counter these systemic risks.
This approach mitigates harm in several key ways:
- Enhanced Competition and Choice: A diversified vendor pool prevents over-reliance on a few large players, fostering competition that drives better service, more transparent pricing, and a greater commitment to finding the right candidate for your specific needs.
- Strengthened Resilience: Building a broad, diverse network of staffing partners creates a more resilient supply chain. If one agency cannot fill a need, you have multiple other avenues, reducing the risk of dangerous coverage gaps.
- Community-Aligned Care: Smaller, community-focused agencies often have a deeper understanding of regional needs and can provide clinicians who are a better cultural and operational fit, leading to more stable placements and higher-quality care.
Choosing to democratize your staffing strategy is not just a procurement decision; it is an ethical one that builds a safer, more sustainable ecosystem for all.
How Syncx Helps Healthcare Organizations Stay on Track
Upholding the duty of non-maleficence in today’s complex staffing environment is a monumental challenge. Syncx was founded to meet this challenge head-on. We are a managed service provider for locum tenens with an explicit mission: to democratize healthcare staffing by empowering a diverse network of agencies, thereby giving you better, more ethical access to the talent you need.
Syncx helps you stay on track with your ethical and operational commitments by providing:
- A Curation of Quality & Safety: We vet and partner with high-performing agencies, ensuring you have access to a pool of pre-qualified talent from a variety of sources, all committed to the highest standards of patient care.
- Simplified, Centralized Management: We act as your single point of contact, managing the complexities of working with multiple agencies. This saves your team invaluable time and reduces administrative burden, allowing you to focus on strategic initiatives rather on vendor management.
- Risk Mitigation Through Diversification: By integrating our diverse network, we build a resilient staffing model for your organization that protects you from the volatility and limitations of a consolidated market. This directly safeguards your patients from the harms associated with sudden, unfillable staffing gaps.
Ready to build a staffing model that truly puts patient safety first?
We invite you to experience the Syncx difference. Let us show you how our democratized approach to locum tenens provides not only greater choice and cost-effectiveness but also a more robust ethical foundation for your organization.
Contact us today for a complimentary consultation on how to fortify your staffing strategy and uphold your commitment to non-maleficence.
