
Technology for Better Workforce Compliance in Healthcare
In the high-stakes environment of healthcare, a single compliance oversight can jeopardize patient safety, trigger massive penalties, and shatter hard-earned reputational trust. Yet, managing workforce compliance is more complex than ever, spanning permanent, contingent, and float pool staff across a labyrinth of regulations.
This article cuts through the complexity, offering healthcare executives and staffing leaders a strategic roadmap. We will explore the foundational pillars of a resilient compliance program and the critical technologies that transform this operational necessity into a competitive advantage.
What is Workforce Compliance in Healthcare?
Workforce compliance in healthcare is the ongoing process of adhering to patient safety regulations and protocols. A large component of compliance is ensuring all staff are qualified, credentialed, and adhere to legal and internal policy standards. It spans from initial hiring (verifying licenses and backgrounds) to maintaining daily adherence to clinical protocols and even incorporating professional development requirements. Ultimately, it mitigates risk, protects patients, and safeguards the organization’s integrity and financial wellbeing.
Compliance is a continuous lifecycle that begins the moment a candidate is considered and extends through their entire tenure with your organization. In today’s environment of heightened scrutiny, labor shortages, and evolving telehealth regulations, a reactive approach to compliance is a significant operational and financial risk.
A robust workforce compliance program directly safeguards your organization against a triad of threats:
- Clinical & Patient Safety Risks: Ensuring only competent, properly credentialed providers deliver care.
- Financial & Legal Risks: Mitigating multimillion-dollar penalties for violations of regulations like HIPAA, Stark Law, and conditions of participation for Medicare/Medicaid.
- Reputational Risks: Protecting the organization’s brand from the devastating impact of compliance failures that erode patient and public trust.
Ultimately, workforce compliance is a critical strategic function that enables scalable growth, protects revenue, and is the bedrock of a high-reliability organization.
Four Pillars of Healthcare Workforce Compliance
To manage the complexity of healthcare workforce compliance, leadership should structure their strategy and technology investments around four core pillars. This framework ensures comprehensive coverage from hiring to daily practice.
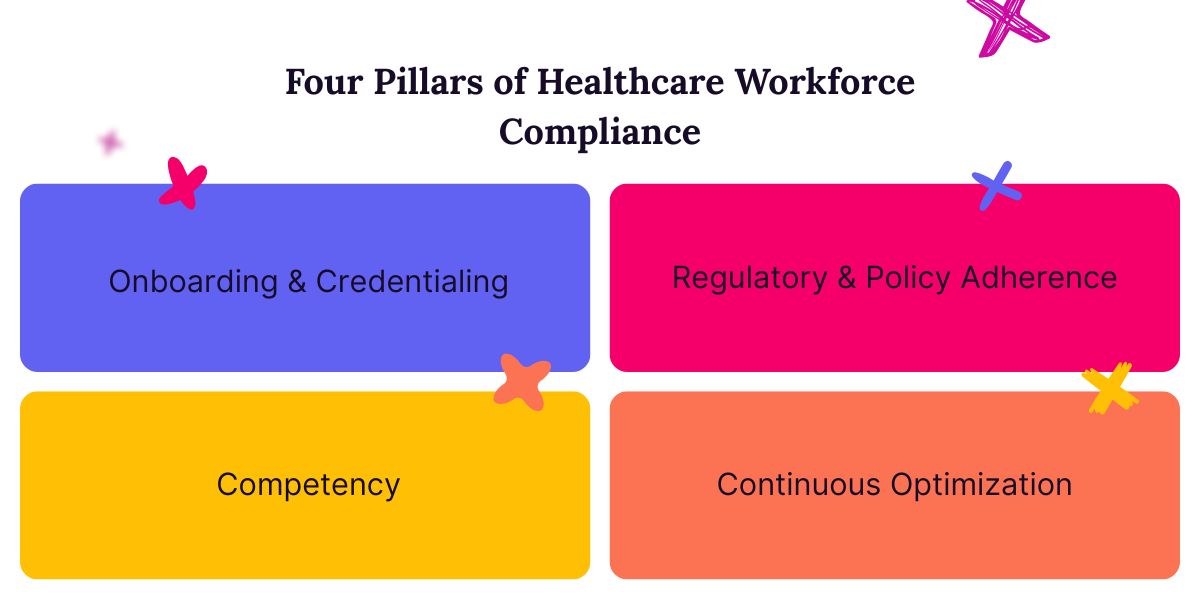
Pillar 1: Onboarding & Credentialing
This is the foundational gatekeeping pillar. Credentialing ensures that every individual granted clinical privileges is who they say they are and has the verified qualifications to perform their duties. This includes primary source verification of licenses, education, board certifications, and work history, as well as conducting criminal background checks and monitoring the OIG exclusion list. Failure here is the single greatest point of failure for a compliance program.
Pillar 2: Competency
This pillar moves from “are they allowed to work?” to “are they able to work safely here?” It encompasses:
- Ongoing Competency: Validating and tracking that staff maintain the skills required for their specific assignments and units.
- Scope of Practice: Ensuring staff are deployed within the strict boundaries of their license and institutional privileges.
- Internal Float Pools: Managing a flexible workforce without sacrificing compliance, by ensuring float staff are properly oriented and credentialed for each unit they support.
Pillar 3: Regulatory & Policy Adherence
This is the pillar of daily operations. It focuses on ensuring that staff actions and workflows comply with the vast array of external regulations and internal policies. Key areas include:
- Licensure & Certification: Tracking renewals and ensuring no one works with an expired credential.
- Health & Safety Standards: Adherence to OSHA, infection control, and safety protocols.
- Data Privacy: Strict compliance with HIPAA and other patient privacy laws in every interaction with patient data.
Pillar 4: Continuous Optimization
A static compliance program is a failing one. This final pillar transforms compliance from a point-in-time audit to a dynamic, proactive process. It involves:
- Audit Trails: Maintaining impeccable records for regulatory bodies.
- Incident Reporting & Analysis: Learning from near-misses and adverse events to strengthen systems.
- Technology Utilization: Leveraging automated systems to continuously monitor license status, track training completions, and analyze data for emerging risks.
By building and reinforcing these four pillars, healthcare organizations can create a resilient compliance infrastructure that not only prevents violations but also fosters a culture of safety and quality.
What Technologies Can Improve Workforce Compliance in Healthcare?
Traditional manual methods of managing workforce compliance are prone to human error, create dangerous latency in verification processes, and consume valuable administrative resources. The strategic integration of targeted technology is now essential for building a compliant, agile, and resilient workforce. The following solutions are organizationally scalable and mitigate significant financial and reputational risk.
Credentialing Monitoring
The cornerstone of any compliance program is the assurance that every clinician possesses valid credentials. But credentialing processes made up of spreadsheets and calendar reminders create critical vulnerabilities that can jeopardize patient safety and accreditation. Modern credentialing monitoring technology directly addresses this by automating the primary source verification and ongoing tracking of professional credentials such as state licenses, board certifications, and DEA registrations.
These platforms function as a centralized system of record, continuously scanning primary sources for status changes and expiration dates. They proactively alert both the individual provider and administrative staff well in advance of a renewal deadline, creating a safety net against human oversight. Furthermore, they provide a complete audit trail for surveyors.
Internal Float Pool
An internal float pool is a powerful tool for managing fluctuating patient census and controlling labor costs that can also help lessen compliance risks by allowing organizations to retain veteran and near-retiring staff. Float pools provide an opportunity for trusted, valuable staff members who want more flexibility and control over their schedule to work in non-traditional roles. They help you reduce reliance on brand new locums providers and thus lessen your compliance risks. In other words, your seasoned GI specialist who is nearing retirement doesn’t need to leave your system completely in order to start winding down their career.
Technology designed for internal float pool management provides a dynamic and compliant framework for mobilizing this flexible workforce. What is more, these systems not only help you keep vital team members that want to leave traditional roles, they do so in a way that can reduce your reliance on locums staffing agencies and lower your contingent staffing costs.
Physician Applicant Tracking System
The journey toward a compliant workforce begins with the submission of an application. A Physician Applicant Tracking System (ATS) distinguishes itself from traditional hiring software through how it addresses compliance risk. This technology centralizes the management of the entire candidate pipeline, from sourcing and communication to the meticulous collection of prerequisite documentation.
By enforcing standardized workflows, an ATS ensures that every candidate for a privileged position progresses through the same rigorous verification checkpoints. It provides a transparent view of each application’s status, highlighting missing documents, incomplete references, or pending verifications. This level of organization prevents crucial compliance steps from being overlooked in a manual process. The system creates a defensible audit trail that demonstrates due diligence from the initial contact, long before a formal credentialing file is ever assembled.
Data Loss Prevention (DLP) Tools
While credentialing and applicant tracking secure the qualifications of the workforce, protecting patient data secures the integrity of their work. Data Loss Prevention tools are vital resources for maintaining compliance with HIPAA and other data privacy regulations. These solutions operate as a vigilant safeguard, monitoring how Protected Health Information is accessed, used, and shared across the organization’s network, endpoints, and cloud environments.
DLP tools are configured with policies that identify and control the movement of sensitive data. They can automatically block a staff member from emailing a patient file to an unsecured personal account, prevent the unauthorized transfer of large datasets to a USB drive, and even redact or encrypt sensitive information before it is shared with an external partner. By proactively preventing both malicious and accidental data breaches, DLP tools reduce the risk of catastrophic regulatory fines and reputational damage.
Learning Management Systems (LMS) with Automated Tracking
A well-trained workforce is a compliant workforce, yet traditional methods of tracking mandatory education are often fragmented and inefficient. A Learning Management System with robust automated tracking transforms regulatory and competency training from an administrative challenge into a measurable, assured outcome. This technology provides a centralized platform for deploying, managing, and documenting all required educational activities, from annual HIPAA and safety certifications to clinical skills updates.
The critical value of an LMS lies in its automation and accountability. The system can automatically assign courses based on role, department, or specific compliance needs, and send escalating reminders until completion is achieved. This eliminates the manual chase for certificates and promotes better completion rates for mandatory training.
VR (Virtual Reality) Clinical Training
Virtual Reality clinical training represents a paradigm shift in how healthcare organizations can ensure and validate that their staff can perform within compliance standards when it matters most. VR creates immersive, realistic clinical environments where providers can practice complex procedures, rare emergency protocols, and delicate patient interactions without any risk to actual patients.
This technology elevates compliance from theoretical knowledge to demonstrated proficiency. It provides objective, data-driven insights into a clinician’s decision-making, technical skill, and adherence to established protocols in a controlled setting. Organizations can use this data to verify competency for credentialing and privileging, ensuring that staff are not merely trained but are truly prepared.
Workforce Compliance for Contingent and Float Pool Staff
Flexible staff members are essential for managing patient volume fluctuations, yet they introduce a heightened level of risk due to their transient nature. A technology-driven approach is not just beneficial but mandatory to ensure every individual, regardless of employment status, meets the same rigorous compliance standards.
Solutions like locum tenens managed services and internal float pools are vital for maintaining compliance. These systems offer seamless ways to promote rapid onboarding, credentialing, and deployment of staff while maintaining a continuous and verifiable chain of compliance, from initial vendor credential verification through to assignment-specific competency validation.
We’re Your Partners in Compliant Locums Staffing
Ensuring a fully compliant workforce in today’s complex healthcare environment requires a partner with the right technology and expertise. Syncx provides a holistic solution with our proprietary Vendor Management System (VMS) and Applicant Tracking System (ATS) designed specifically for the unique demands of healthcare staffing, empowering you to mitigate risk, streamline operations, and focus on delivering exceptional care.
Schedule a demo today to see how our managed services can secure and optimize your contingent labor program.