Every healthcare professional knows the drill: A sudden surge in patients. A wave of staff call-outs. The frantic scramble to fill shifts without blowing the budget or compromising care. In today’s unpredictable healthcare environment, managing contingent labor isn’t just administrative work. It’s a strategic imperative.
That’s where Vendor Management Systems (VMS) and Managed Service Providers (MSP) come in. These solutions promise to bring order to staffing chaos, but with one key difference: A VMS gives you the tools to manage temporary labor, while an MSP relies on experts together with technology to handle the entire process for you. The choice between them (or the decision to combine both) can transform how your organization scales, saves, and sustains quality care.
In this article, we’ll break down how VMS and MSP models actually work in healthcare settings, when each solution makes sense (and when you need both), and the emerging trends reshaping contingent workforce management. Whether you’re drowning in agency invoices, struggling with fill rates, or just curious about optimizing your staffing strategy, this guide will help you navigate your options with confidence.
What Is the Difference Between a VMS vs. MSP in Staffing?
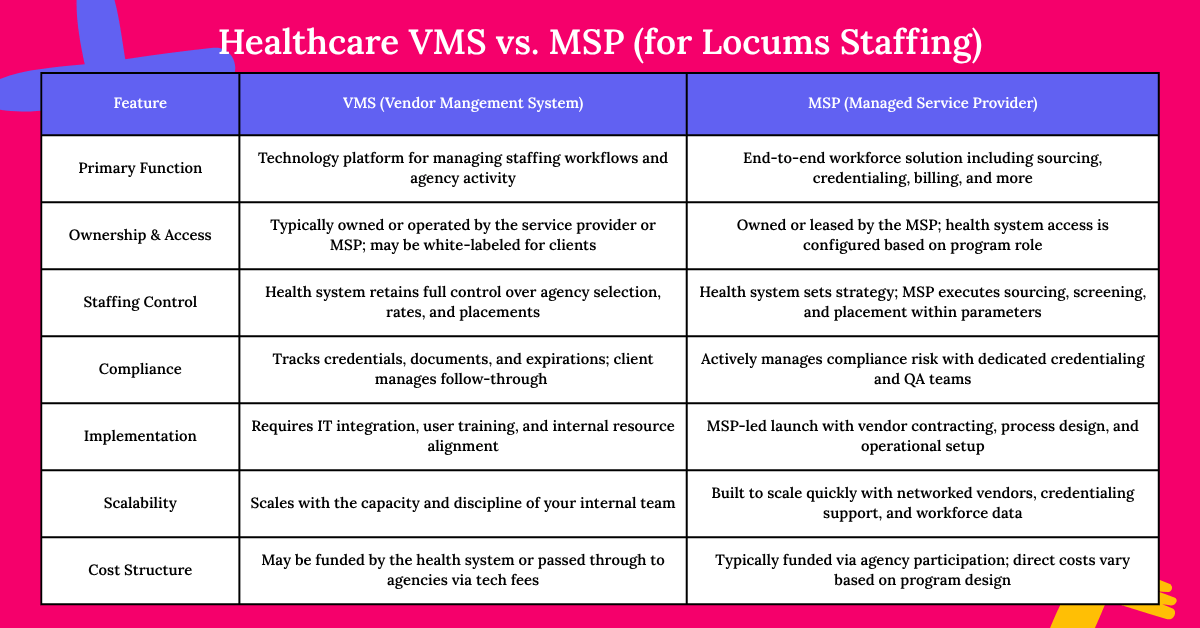
A Vendor Management System (VMS) is the technology that helps healthcare organizations manage contingent labor, while a Managed Services Provider (MSP) is the service that oversees the entire staffing process. In other words, a VMS is the software platform that tracks vendors, approvals, and spending, while an MSP is the outsourced team that uses that technology (and more) to source, onboard, and manage your temporary workforce. Here’s how they compare across key areas:
Ownership & Management
- VMS: A software platform that acts as a digital hub for managing contingent labor. A technology company, MSP organization or VMS provider owns the technology.
- MSP: A third-party service provider (like Syncx or AMN Healthcare) that takes full responsibility for managing temporary and contingent staffing—from sourcing to onboarding to payroll. Some MSPs (like Syncx or AMN Healthcare) either develop their own VMS technology, lease it, or white-label an existing platform to support the staffing program. In rare instances, a health system may license or white-label a VMS directly, but this still typically involves outside support for configuration, integration, and day-to-day administration.
Staffing Control
- VMS: You stay in control. Your team manages vendor relationships, selects candidates, approves shifts, and sets priorities—using the VMS as your operational hub. This model is best suited for organizations with dedicated internal resources and strong staffing discipline. The VMS gives you visibility and structure, but your team still drives the execution.
- MSP: You set the strategy, the MSP runs point. A good locums MSP operates within your defined parameters—like rate caps, quality standards, and credentialing requirements—but takes on the day-to-day work of sourcing, vetting, and filling roles. You retain ultimate authority, but the MSP brings consistency, speed, and expertise to the front lines. Ideal for systems looking to scale without expanding internal headcount.
Compliance
- VMS: Acts as your digital compliance auditor. It flags expired licenses or missing certifications but relies on your staff to resolve issues.
- MSP: Serves as your proactive compliance officer. They manage the details of licensing, credentialing, and privileging to ensure every provider and agency knows what’s needed, when it’s needed, and will close loops to ensure you don’t have to.
Implementation
- VMS: Implementing a VMS for locums staffing does require IT coordination and internal buy-in, particularly around credentialing, timekeeping, and billing workflows. While many platforms can technically be stood up in weeks, a realistic implementation timeline is 60–90 days for full functionality. You’ll also need internal staff—usually from HR, procurement, or medical staff services—to manage the platform and vendor relationships over time.
- MSP: A locums MSP offers more of a turnkey solution, typically standing up in 30–60 days, depending on contract complexity and system readiness. The MSP not only manages the platform (whether proprietary or leased) but also handles vendor contracting, process design, reporting setup, and go-live support. Internal resources are still required, but the lift is significantly lighter, especially long-term.
Scalability
- VMS: Scalability depends on your internal resources and processes. The VMS provides the infrastructure to manage more volume, more vendors, and more data—but it’s only as fast and flexible as the team running it. For health systems with a mature internal staffing function, a well-implemented VMS can support meaningful scale while maintaining control and visibility.
- MSP: MSPs are purpose-built to scale—especially during high-demand periods or system-wide expansion. With access to broad multi-vendor networks, pre-established rate frameworks, and credentialing teams on standby, a good MSP can quickly absorb volume spikes, ramp up in new geographies, or stand up specialty coverage in weeks, not months. The infrastructure is already in place; your system benefits from it instantly.
What is the Role of a VMS in Healthcare?
A Vendor Management System (VMS) acts as the central command center for managing contingent healthcare staffing. It brings structure and visibility to what is often a fragmented, manual, and compliance-heavy process—especially when juggling multiple agencies and shift-based needs.
At its core, a VMS digitizes and streamlines critical workflows:
- Requisitions (a.k.a. Jobs) route through predefined approval chains.
- Agency submissions are centralized for easy tracking.
- Credentials are verified in-platform before a provider steps foot on site.
The real power of a VMS is in what it reveals. With real-time dashboards and customizable reporting, it surfaces insights on spend, utilization, fill rates, and agency performance—giving leaders the data they need to take action faster and smarter.
But let’s be clear: a VMS isn’t a staffing team in a box. It doesn’t replace human strategy or decision-making—it amplifies it. Success with a VMS still requires engaged, knowledgeable users who can interpret the data, hold agencies accountable, and move quickly when needs arise.
That’s why many health systems choose to pair their VMS with a managed service partner (MSP)—combining tech-driven efficiency with expert execution.
What is the Role of an MSP in Healthcare?
If a VMS is the tool, a Managed Services Provider (MSP) is the expert using it to deliver results. An MSP brings operational strength, strategic insight, and healthcare-specific know-how to transform contingent staffing from a reactive fix into a forward-looking workforce solution.
An MSP acts as an extension of your internal team—handling the complexities of sourcing, onboarding, and managing temporary providers across departments or facilities. But their impact goes well beyond logistics.
Before a job is ever posted, an MSP is already at work:
- Analyzing historical staffing data
- Forecasting future coverage gaps
- Building and maintaining networks of qualified vendors and clinicians
When census spikes hit—whether from a seasonal surge, provider burnout, or unexpected vacancies—your MSP helps you respond with speed, quality, and cost control. They enforce rate discipline, ensure credentialing compliance, and maintain provider continuity across shifts, sites, and specialties.
But what really sets a healthcare MSP apart is alignment. A good partner doesn’t just fill jobs—they help you:
Reduce dependence on high-cost agencies
- Improve fill rates and time-to-start
- Navigate credentialing and labor regulations
- Support clinical quality through smarter provider deployment
In short, an MSP helps turn your contingent labor strategy into a competitive advantage—fueling better care, lower costs, and a stronger workforce.
How Do a VMS and MSP Work Together?
A VMS and MSP aren’t competing models—they’re complementary. When paired effectively, they form a seamless workforce engine: the VMS provides the infrastructure, and the MSP brings the strategy and execution muscle.
The VMS acts as the system of record—automating workflows, centralizing data, tracking compliance, and giving stakeholders visibility into every requisition, submission, credential, shift, and invoice.
The MSP uses that infrastructure to:
- Source and screen providers
- Manage vendor performance
- Negotiate rates and terms
- Drive consistent fill and quality
When a department requests urgent locum coverage, the MSP activates its vendor network, finds qualified providers, and negotiates aligned rates. Meanwhile, the VMS routes the request, captures all submissions, verifies credentials, manages documentation, and ensures shifts and costs are tracked in real time.
As the assignment plays out, the VMS collects rich data on fill rates, bill rates, and performance. The MSP then uses that data to optimize sourcing strategies, adjust agency tiers, and flag upcoming gaps—before they become critical.
How to Choose Between a VMS and MSP (or Both)
Choosing between a VMS, an MSP, or the combination of both comes down to three key questions:
- What problem are you solving?
- Who will manage the process day to day?
- How much control do you want to retain?
If you already have strong agency relationships, solid fill rates, and internal teams with capacity to manage workflows, a standalone VMS might be the right fit. It gives you the technology backbone to digitize processes, gain visibility, and enforce consistency—without handing off control.
But if your team is stretched thin—or if you’re facing rising costs, spotty coverage, compliance risk, or lack of standardization—a Managed Services Provider (MSP) brings the strategic lift to stabilize and scale your program.
For many health systems, the combination delivers the best of both worlds.
- The VMS manages the heavy lifting—approvals, documentation, billing, and analytics.
- The MSP focuses on outcomes—agency alignment, clinical fit, speed to fill, and cost control.
Example: A multi-hospital network might use an MSP to standardize staffing operations across facilities, while the VMS enforces those policies and tracks every shift, credential, and dollar in real time.
Start by auditing your pain points:
- Are you buried in spreadsheets?
- Spending too much time on credentialing or invoices?
- Dealing with late fills, inconsistent rates, or siloed processes?
Your answers will point to the solution—whether that’s technology, expert support, or the power of both working in tandem.
Future Trends in Healthcare MSP’s and VMS’s
The healthcare staffing landscape is shifting fast—and MSPs and VMS platforms are no longer just tools for managing locums or temp labor. They’re becoming strategic workforce platforms that help health systems manage all types of provider staffing: permanent, per diem, and everything in between.
Here’s what’s ahead:
Expanded MSP Scope
Modern MSPs are now offering permanent hiring support, float pool management, and even direct engagement models—where they build and manage pools of pre-vetted clinicians who work directly with the health system. This reduces reliance on third-party agencies, cuts costs, and improves provider continuity.
Internal Locums & Float Optimization
Health systems are leaning into internal float pools and in-house locums models, using the VMS to match known providers to open shifts before going to external agencies.
Smarter, Predictive Technology
AI and predictive analytics are helping VMS platforms forecast shortages, optimize rate negotiations, and flag at-risk assignments—before they cause gaps in care.
Data-Driven Performance Management
Health systems are using MSPs and VMSs to hold agencies accountable for key KPIs like time-to-fill, credentialing accuracy, and provider quality—driving higher performance and lower cost over time.
Integrated Tech Ecosystems
VMS platforms are being integrated with credentialing software, HRIS, EHRs, and billing systems to eliminate silos and reduce administrative friction.
Bottom line
Healthcare MSPs and VMSs are no longer just about filling shifts—they’re helping systems build a resilient, right-sized workforce that can flex with demand, reduce agency overuse, and align staffing strategy with patient care goals.
Try a Managed Service Partner for Locum Tenens
If you’re still juggling spreadsheets, scrambling for last-minute coverage, or wondering if you’re overpaying for temporary physicians, it might be time to experience what a true healthcare-focused MSP can do. Syncx MSP specializes in locum tenens staffing that actually understands clinical workflows—not just filling slots, but ensuring the right providers are in place to maintain care continuity.
Why keep wrestling with staffing chaos? See the difference when technology and expertise work together. Schedule your Syncx MSP demo today and discover how you could save 20-30% over agency rates while gainin
