
How to Make Sense of Locums Rates in 2026: A Guide for Hospital Leaders
For many healthcare executives, locums tenens rates can feel like a frustrating black box of sticker shock, unpredictable fluctuations, and a nagging uncertainty about whether you’re getting true value for your investment. Simply accepting these costs as a necessary evil is a strategic misstep. This guide is designed to empower you with clarity and control.
We will deconstruct the factors influencing locums rates, provide a framework for calculating their true return, and outline actionable strategies to optimize your program so you can transform this significant expenditure into a managed, strategic asset for your organization.
Cost Components in Locums Rates
Viewing a locums quote as a simple fee-for-service transaction is a common pitfall. In reality, it is a bundled price for a comprehensive service that addresses a critical operational gap. This section deconstructs that quote, explaining the powerful market forces at play and the specific cost components that, when understood, transform locums from a perplexing expense into a strategic, justifiable investment.
Why Are Locums Rates So High, and Why Do They Keep Increasing?
Locums rates are a direct reflection of the fundamental economic principles of supply and demand, amplified by unique pressures within the healthcare landscape. The primary driver is a severe and persistent physician and advanced practice provider shortage, which has been exacerbated by widespread burnout and an aging workforce retiring early or reducing their hours. This shrinking supply is chasing an ever-increasing demand for clinical services from an aging patient population.
Consequently, locums providers, who represent a finite and highly mobile pool of talent, possess significant pricing power. They can command premium rates because healthcare organizations are competing for their services in a seller’s market, often to keep revenue-generating services open or to avoid costly staff burnout.
Furthermore, the rates are not static; they continue to increase due to inflationary pressures on travel and housing, as well as the rising cost of malpractice insurance. However, the most significant upward pressure comes from the strategic value locums provide. For a hospital or health system, the cost of a vacant position (in terms of lost procedure revenue, cancelled clinic appointments, and excessive overtime payments to core staff) often far exceeds the investment in a locums provider. Agencies and clinicians are keenly aware of this calculus. As the financial and operational impact of vacancies becomes more acute, organizations are willing to pay more to secure coverage, creating a competitive bidding environment that continuously pushes the market rate higher.
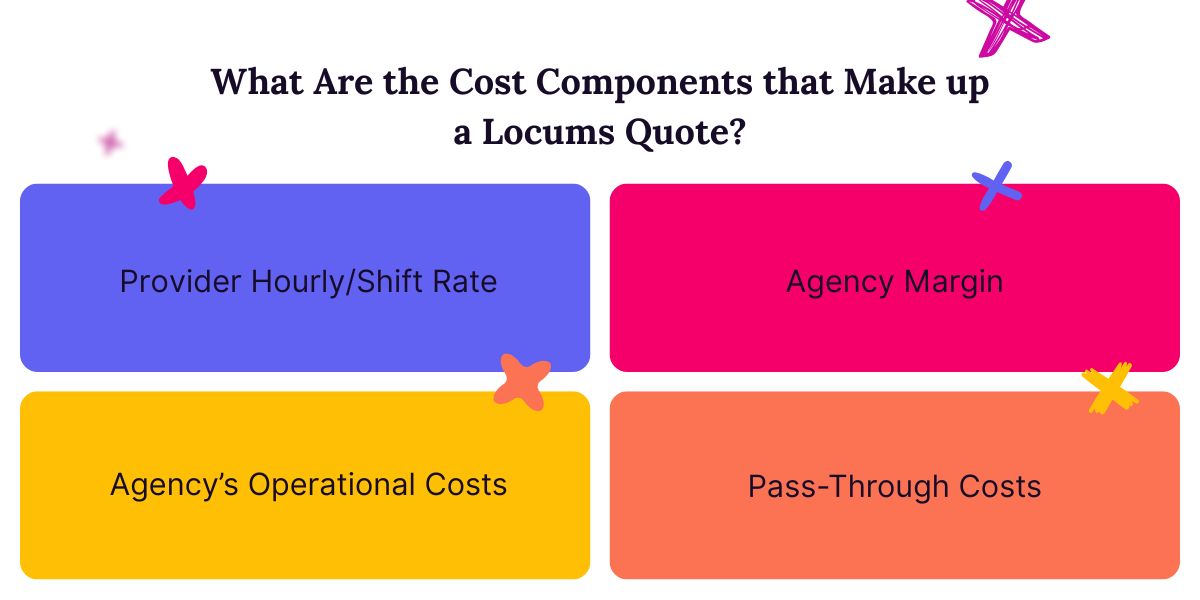
Beyond The Hourly Or Daily Rate, What Are the Cost Components that Make up a Locums Quote?
A locums quote is far more than a clinicians’s paycheck. It is an all-inclusive package designed to deliver a fully vetted, credentialed, insured, and transported professional to your facility with minimal administrative burden on your team. The largest component is typically the clinicians’s pay rate, which is their direct compensation for clinical work.
However, this is just the starting point. The agency markup is layered on top to cover the agency’s operational costs and profit margin. This margin funds their extensive recruitment efforts, sophisticated credentialing and compliance teams, and 24/7 support, which collectively remove a significant administrative burden from your HR and medical staff offices.
Beyond these two core elements, the quote includes a suite of direct pass-through costs. These are often the most misunderstood parts of the quote. They include malpractice insurance premiums, which are essential for risk mitigation and can be substantial for high-risk specialties. Travel and lodging expenses are also factored in, covering airfare, rental cars, and hotel accommodations for the assignment duration.
Additionally, quotes often include fees for licensing and credentialing support, such as securing state medical licenses or hospital privileges, which can be a time-consuming and expensive process if handled internally.
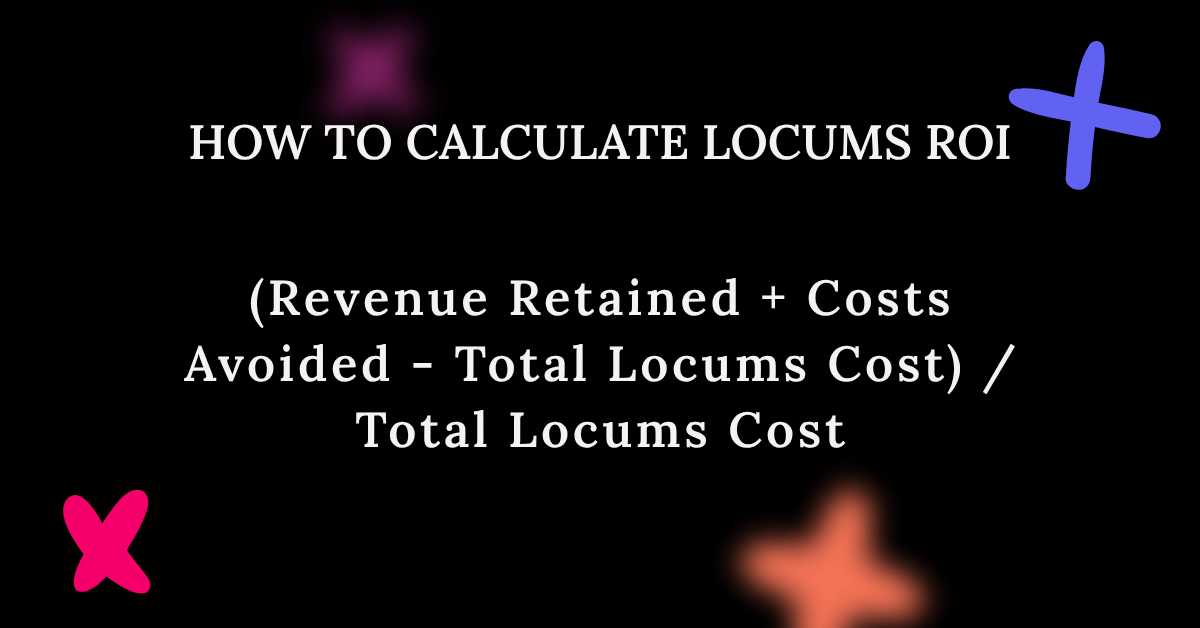
How Do We Calculate the ROI of a Locums Provider?
Calculating the true ROI of a locums provider requires looking beyond the invoice amount and quantifying both the revenue preserved and the costs avoided. A simple but powerful ROI formula starts with the Revenue Retained by keeping a service line or facility open (for instance, the collections from patient visits, surgeries, or procedures that would have been lost or referred elsewhere). To this, you add the Costs Avoided, such as the overtime payments to core staff covering the gap, penalties for cancelled surgical slots, or losses from diverted ambulances. The ROI is then calculated as: (Revenue Retained + Costs Avoided – Total Locums Cost) / Total Locums Cost.
Keep in mind, however, that qualitative factors also have tangible financial consequences. For example, a locums provider can help prevent staff burnout and turnover among your permanent team. The cost of recruiting, onboarding, and training a single new physician can run into the hundreds of thousands of dollars, a significant expense that a locums can help avert. Furthermore, by maintaining patient access and continuity, you protect patient satisfaction scores and market share, which directly impact long-term revenue and reimbursement in value-based care models.
What Is the Financial Impact of a Vacant Position Versus Filling It with a Locums Tenens Provider?
A vacant position represents a direct leak in revenue generation. An unfilled cardiologist, for instance, isn’t performing lucrative procedures; an empty primary care slot isn’t managing a patient panel. This lost revenue can quickly dwarf the cost of a locums. Simultaneously, the vacancy creates increased variable costs. Your organization is likely paying substantial overtime to nurses, technicians, and advanced practice providers to compensate, leading to fatigue and dissatisfaction.
The vacancy not only loses money but also actively erodes your organizational infrastructure by overburdening your permanent staff. This leads to higher turnover, creating a vicious cycle of more vacancies and recruitment costs.
Are There “Hidden Costs” of Using Locums that We Should Be Accounting for in our Financial Models?
Yes, while the direct costs of a locums are clear, astute financial models account for several indirect or “hidden” costs to ensure a complete picture. The most significant is the internal resource cost of onboarding and support. Your administrative, IT, and clinical staff spend considerable time granting system access, providing orientation, and integrating the temporary provider into workflows. This is time not spent on other strategic initiatives.
Furthermore, there can be a productivity and efficiency drag; a locums, unfamiliar with your EMR and facility protocols, may not initially see patients at the same pace as a long-term team member, potentially slightly reducing the volume and revenue they generate.
To mitigate these costs, proactive management is key. Factor in an allocation of internal HR and IT time into your budget. More importantly, you can minimize these hidden costs by optimizing your own processes. Streamlining onboarding with checklists and dedicated points of contact, creating brief but effective facility orientations, and providing “cheat sheets” for your EMR can dramatically reduce the productivity ramp-up time.
Negotiating and Working with Vendors
Understanding the composition of locums rates is only half the battle; the next step is leveraging that knowledge to build effective and cost-efficient vendor relationships. A strategic approach to sourcing and negotiation is what separates organizations that simply pay market rates from those who actively shape their locums expenditure. This involves forming partnerships based on mutual value, clear expectations, and data-driven decisions. The following strategies will empower you to secure the best possible talent at the most responsible rate.
How Can We Negotiate Better Rates Without Sacrificing Quality or Eliminating Good Candidates?
Effective negotiation in the locums market is less about haggling over a single bill rate and more about leveraging strategic models that fundamentally change your purchasing power. The most impactful step is partnering with a vendor-neutral Managed Service Provider (MSP).
An MSP acts as your single point of contact, managing a curated network of agencies on your behalf. This model creates inherent competition, as multiple agencies must submit their best candidates and most competitive rates into a centralized platform to win your business. This eliminates the scenario of you competing against yourself and provides full transparency, allowing the MSP to negotiate from a position of strength and data, all while ensuring you see a wider pool of qualified talent without sacrificing quality.
Beyond the MSP model, developing an internal float pool is a powerful long-term strategy for reducing external locums dependency. By creating a roster of credentialed, internal clinicians who can flex across different facilities or units, you create a first-line, cost-effective defense against vacancies. These internal resources are typically paid at a standard rate, avoiding the premium margins of external agencies.
Should We Work with Multiple Agencies or Have a Primary Vendor?
Working with multiple agencies creates immediate competition, which can theoretically drive down rates in the short term. It gives you access to a larger pool of candidates and can be useful for hard-to-fill specialties or one-off needs. However, this model has significant downsides. Agencies have little incentive to invest time in understanding your unique culture or long-term needs, leading to a transactional relationship. More critically, you can inadvertently create a bidding war against yourself if multiple agencies submit the same candidate, damaging your reputation and inflating the rate.

Conversely, establishing a Managed Service Provider (MSP) or primary vendor partnership shifts the dynamic from competition to collaboration. In this model, you grant a single agency (or a managed program with a few vetted partners) exclusive or preferred access to your locums needs.
The impact on rates is profoundly positive over the long term. Your MSP will act as an extension of your team, providing valuable market data and helping with strategic workforce planning. This partnership approach reduces internal administrative overhead, improves fill rates, and typically results in more stable, predictable, and ultimately lower total costs, even if the bill rate for a single assignment may not always be the absolute lowest on the market.
The Long-Term Impacts of Locums
While locums tenens are an indispensable tool for managing immediate staffing gaps, healthcare leaders must vigilantly monitor their long-term organizational impact. Used tactically, locums provide stability and breathing room.
At What Point Does Relying on Locums Become a Strategic Liability Instead of a Tactical Solution?
Reliance on locums transitions from a tactical solution to a strategic liability when it becomes a permanent substitute for a sustainable workforce strategy. Key indicators include when locums expenditure is no longer a variable, unpredictable cost but a cemented, growing line in the operational budget, or when core clinical services are perpetually dependent on temporary staff to remain open.
What Internal Factors Force Reliance on Locums?
An over-reliance on temporary staff is frequently a symptom of deeper, systemic issues within the healthcare organization itself. Identifying and addressing these internal drivers is the most effective way to reduce dependency and control long-term contingent labor spending. The primary culprits often lie in a slow physician recruitment lifecycle, bureaucratic internal processes, and cultural challenges that affect retention.
When the timeline from identifying a need to extending an offer stretches for months, the resulting vacancy must be filled temporarily to maintain services. This is compounded by a cumbersome credentialing and privileging system. Furthermore, underlying cultural and retention issues create a vicious cycle that perpetuates locums dependency. High burnout and turnover among permanent staff directly increase vacancy rates, constantly creating new gaps that require temporary fill-ins.
Finally, an inefficient or non-existent internal float pool leaves no flexible, cost-effective internal resource to manage fluctuations in demand or short-term absences, defaulting the solution to the external locums market every time. By diagnosing these internal factors, leaders can shift from perpetually funding a symptom to finally curing the disease.
Optimize Your Contingent Physician Staffing Program Today
Ready to move from reactive spending to strategic workforce management? Stop letting unpredictable locums costs dictate your budget and compromise your long-term goals. Partner with Syncx for a data-driven, partnership approach that delivers premium talent at sustainable rates, streamlines your credentialing and onboarding to reduce dependency, and provides the strategic insights you need to build a more resilient and cost-effective physician staffing model.
Book a demo today to see how we can transform your largest staffing challenge into a measurable competitive advantage.