The compounding pressures of the last few years have accelerated a silent healthcare workforce crisis from a simmer to a rolling boil, forcing a fundamental re-examination of how we support, manage, and value clinical talent. We’re moving into an era of profound transformation defined by technological disruption, evolving care models, and a non-negotiable demand for well-being.
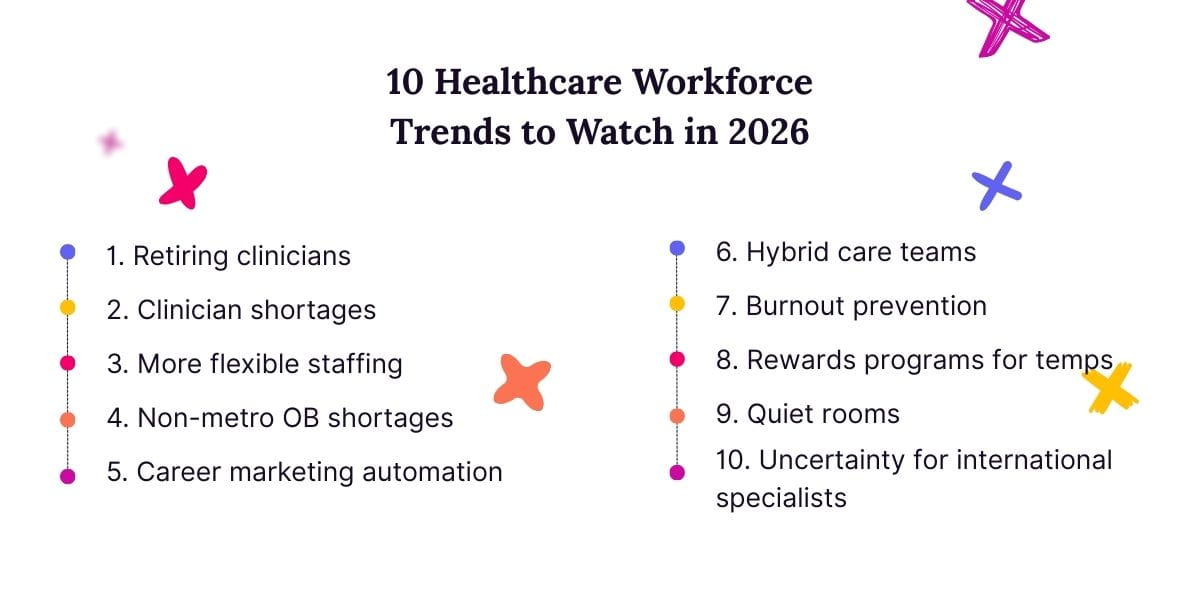
In this landscape, staying ahead is an operational imperative. This blog dives into 10 critical trends set to define the healthcare workforce in 2026, providing a roadmap for leaders ready to build a more agile, sustainable, and resilient future. From the strategic integration of AI to the urgent need to combat burnout and stabilize a volatile staffing market, we break down the forces that will shape the next year as well as what your organization can do to not just navigate them, but to lead.
Let’s get started.
1. An Aging Workforce Continuing Toward Retirement
The healthcare sector in 2026 will confront the accelerated and mass retirement of the Baby Boomer generation. According to research from the National Academy of Sciences, the number of healthcare workers over 60 doubled between 2000 and 2020. As these individuals age into retirement, it will disproportionately affect senior clinical roles, including seasoned staff nurses, nurse managers, and specialist physicians, who possess decades of nuanced, practical judgment that is irreplaceable by protocols or technology.
For many organizations, this exodus will necessitate a shift in knowledge management and succession planning. Forward-thinking health systems will aggressively implement formalized “knowledge capture” programs well before retirement dates, using methods like mentoring partnerships, video-recorded procedural demonstrations, and structured interviews to document the tacit knowledge that veteran clinicians hold. Furthermore, to mitigate the brain drain, organizations will be forced to create more attractive “phased retirement” models and part-time clinical or advisory roles utilizing tools like float pools.
2. Nursing and Physician Shortages
The nursing and physician shortages will intensify in 2026, evolving from a generalized workforce gap into acute, strategic crises concentrated in specific high-stakes domains. The American College of Physicians predicts a shortage of 85,000 physicians by 2036. Similarly, the National Center for Health Workforce Analysis projects that we would need more than 78,000 Registered Nurses to cover the shortage by the end of 2025..
In response, the solution will no longer be focused solely on recruiting more individuals but on fundamentally rethinking care delivery models to maximize the impact of every clinician. This will involve a massive and intentional “scope of practice expansion” for Advanced Practice Registered Nurses (APRNs) and Physician Assistants (PAs), empowering them to manage a greater share of patient care independently, especially in underserved areas. Additionally, healthcare systems will increasingly rely on team-based care, where physicians act as overseers and consultants for a team of NPs, PAs, nurses, and medical assistants, thereby leveraging the physician’s expertise across a much larger panel of patients.
3. Non-metro OB shortages
While much workforce discussion centers on broad physician and nursing shortages, one of the most acute and geographically concentrated crises is in maternal care. A stark disparity already exists and will continue to grow between urban and non-metropolitan areas in access to obstetric and gynecological (OBGYN) services. According to the Bureau of the Healthcare Workforce, non-metro areas face a 46% shortage of OBGYNs by 2038. This deficit creates “maternity care deserts,” leaving millions without local access to essential prenatal, delivery, and women’s health services. The problem is projected to be most severe in high-population states with large rural regions, with Texas, California, and Florida expected to face the highest absolute shortages.
This shortage directly correlates with worsening maternal health outcomes, including higher rates of maternal mortality and morbidity in rural communities. Patients often must travel hours for routine care or face delayed interventions. In response, healthcare systems are deploying innovative solutions like telehealth integration, retention incentives, and partnerships with staffing agencies that specialize in women’s health providers.
4. Expanded Internal Flexible Staffing Models
In direct response to the volatility and high cost of the external staffing market, leading healthcare organizations will aggressively develop and expand internal flexible staffing models in 2026. These models function as an internal “gig economy,” creating pools of pre-credentialed, vetted clinicians that include part-time employees, retirees, and those seeking non-traditional schedules. With the right software, staff can be deployed dynamically across the system based on real-time need.
The strategic implementation of these models will become a key differentiator for attracting and retaining top talent. By offering more flexible scheduling options to near-retiring staff and people seeking more work-life balance, organizations can cater to the diverse needs of a multigenerational workforce. When done well, internal flexible models create a win-win: clinicians gain autonomy over their careers, and health systems build a resilient, adaptable workforce that can weather fluctuations in patient volume without sacrificing financial stability or care standards.
5. Career Marketing Automation
Facing a perpetual talent shortage, forward-thinking healthcare systems will embrace career marketing automation, treating potential candidates like valued customers throughout a prolonged nurturing journey. This involves using automated CRM platforms to segment talent pools (from students and passive job seekers to former employees) and deliver personalized, targeted content via email, text, and social media. A nursing student might receive information about a system’s residency program, while a seasoned nurse who previously applied might get an alert about a new flexible scheduling option or a signing bonus for a specific specialty they’re certified in, keeping the organization top-of-mind.
This automated, always-on engagement strategy will become crucial for building a robust talent pipeline and reducing time-to-hire. Instead of launching expensive, broad-scope campaigns only when a crisis hits, organizations will continuously build relationships and brand loyalty with potential applicants, so when they are ready to make a move, that health system is the first they think of.
6. Expanded Hybrid Care Teams
The concept of the care team will increasingly include a hybrid model that seamlessly blends in-person and virtual clinicians to maximize efficiency and expertise. We will see the formalization of roles like “virtual nurses” who remotely manage patient admissions, discharges, and education for a full floor of patients, and “tele-ICU” clinicians who provide constant monitoring and support for critical patients across multiple facilities.
This expansion will redefine traditional clinical roles and create new, specialized career paths within healthcare. It allows experienced clinicians who may be unable to withstand the physical demands of bedside care (due to injury, age, or disability) to continue practicing in a high-impact virtual capacity, retaining their invaluable expertise within the workforce. For the on-site team, the virtual layer acts as a powerful force multiplier, handling administrative tasks and providing expert oversight, which reduces the cognitive load on bedside nurses and allows them to focus on hands-on, compassionate patient care.
7. Systemic Efforts to Combat Burnout
The healthcare industry is beginning to recognize that burnout is not a personal failing but an operational and cultural problem requiring structural solutions. This will manifest in the widespread adoption of technology designed to reduce cognitive load and administrative burden, such as ambient AI scribes that automate clinical documentation and streamlined EHR interfaces.
The second prong of this effort will focus on creating cultures of psychological safety and sustainable practice. This means not only offering Employee Assistance Programs (EAPs) to integrating mental health support directly into the workflow, such as providing access to on-demand therapists specializing in clinician trauma and establishing peer-to-peer support networks that are destigmatized and promoted by leadership. Organizations are also likely to become more creative with scheduling, offering more non-clinical days for administrative tasks, professional development, or simply rest.
8. Expanded Rewards Programs for Temporary Positions
In 2026, the competition for temporary clinical talent will intensify, forcing healthcare organizations to adopt more sophisticated, loyalty-based rewards programs traditionally reserved for permanent employees. Recognizing that a transient workforce is both costly and disruptive, more organizations will start to investigate structured programs for their per-diem, internal pool, and even external agency staff to incentivize consistency and reliability, including things like awarding points for completing shifts that can be redeemed for gift cards or other purchases.
This strategic expansion will aim to cultivate a stable “regular temporary” workforce, reducing over-reliance on unknown external agency staff. By offering tangible, accumulated benefits, organizations give temporary staff a compelling reason to choose their facility repeatedly over others, fostering a sense of connection and investment even without a permanent contract.
9. Quiet Rooms (and Other Mental Healthcare Benefits)
“Quiet Rooms,” or dedicated spaces where staff can rest throughout the day, are an efficient way for organizations to demonstrate a broader institutional commitment to mental well-being. We expect to see even more of these intentionally designed sanctuaries built with evidence-based principles in mind: soundproofed walls, calming lighting (e.g., circadian rhythm-friendly), comfortable seating, and elements of biophilia (like living walls or nature sounds) to provide a genuine cognitive escape from the high-stimulus clinical environment.
10. Uncertainty for International Specialists
The year 2026 will see heightened uncertainty for international healthcare specialists (e.g., physicians, nurses, physical therapists) due to a perfect storm of geopolitical tensions, evolving immigration policies, and domestic protectionist pressures. While many developed nations face acute staffing shortages, political rhetoric and policy changes often swing unpredictably, creating a volatile environment for visa approvals, renewals, and pathways to permanent residency.
This climate of uncertainty creates a significant strategic risk for healthcare organizations that rely on this talent pool to fill critical specialty gaps, particularly in underserved areas. Long and unpredictable visa processing times can lead to last-minute rescinded job offers, leaving vital positions unfilled and disrupting care continuity. For the international specialists themselves, this environment may lead to increased anxiety, burnout, and a decision to seek opportunities in more politically stable countries—or return home—thereby depleting a crucial talent pipeline.
FAQs about Healthcare Workforce Trends
Is the healthcare workforce shrinking?
The number of open roles in healthcare is not shrinking, but the number of available professionals to fill them is. A mix of factors contribute to these shortages, including an aging workforce, a lack of educational recruits, and fewer professionals coming from overseas.
What is the fastest growing healthcare occupation?
According to McKinsey & Co, the fastest growing healthcare sector is software technology, driven by organizations looking for increasingly efficient ways to do business and greater investments in generative AI.

Why are healthcare workers so burnt out?
Healthcare worker burnout is a complex issue caused by a combination of systemic, cultural, and personal factors:
- Overwhelming Workloads and Administrative Burden: Many healthcare workers are responsible for too many patients at once, which compromises their ability to provide safe, quality care and leads to moral distress. Furthermore, a staggering amount of their time is consumed by documentation, charting, and navigating complex Electronic Health Record (EHR) systems.
- Moral Injury and Ethical Strain: Healthcare workers enter their fields to heal and help people. Moral injury occurs when they are repeatedly placed in situations where they cannot provide the standard of care they know is right due to constraints beyond their control, like lack of time, resources, or staffing.
- Emotional Toll and Trauma: Healthcare professionals routinely witness human suffering, trauma, death, and grieving families. They are expected to manage their own emotions while providing compassionate care, which can lead to compassion fatigue.
- Lack of Autonomy and Control: Many healthcare workers feel like cogs in a machine. Their schedules, workflows, and decisions are often dictated by hospital policies, insurance requirements, and productivity metrics rather than their own clinical judgment. This loss of control over their work environment is a significant contributor to feelings of helplessness and burnout.
- Inadequate Support and Resources: This includes everything from insufficient staffing and broken equipment to a lack of support from leadership. When workers constantly have to “do more with less,” it creates a perpetual cycle of stress.
Next-Level Tools for Managing a Healthcare Workforce
The trends are clear: volatility is the new normal, and traditional staffing methods are no longer enough. To navigate the complexities of 2026, you need a partner that provides both cutting-edge technology and deep industry expertise.
Syncx offers more than just access to locum tenens and temporary staff; we provide a sophisticated managed services platform designed for stability and intelligence. Our system gives you real-time visibility into your entire workforce, predictive analytics to forecast needs, and the expert support to seamlessly integrate top-tier clinical talent, all while controlling costs and reducing administrative burden.
Stop reacting to staffing crises and start building a resilient, agile workforce. Book your demo today and see how Syncx delivers the next-level tools and strategic partnership you need to thrive.

