Hospitals face a relentless balancing act: delivering exceptional patient care while managing unpredictable staffing needs. Seasonal surges and unexpected absences lead to gaps in coverage that can strain budgets, overburden teams, and even impact patient outcomes.
Float pools are an agile, cost-effective staffing solution that keeps operations running smoothly. More than just a stopgap, a well-designed float pool acts as a strategic asset—optimizing resources, reducing reliance on expensive agency staff, and ensuring continuity of care across every unit.
In this article, we’ll explore how float pools work, why leading hospitals rely on them, and how innovative tools like Syncx Float Pool transform this model into a scalable competitive advantage. Whether you’re evaluating your first float pool or seeking to optimize an existing one, the right approach can turn staffing challenges into opportunities—for your bottom line, your teams, and your patients.
What Is a Float Pool in a Hospital?
A float pool is a flexible team of healthcare professionals—like physicians, advanced practice providers, CRNAs, and nurses—who are available to work across multiple departments and teams. Unlike staff assigned to a single unit, float pool members “float” to areas with the greatest need in order to meet fluctuations in demand, staff shortages, or unexpected absences.
Float pool management often involves a software solution to create and fill shifts across the hospital. These platforms integrate with the hospital’s staffing and scheduling systems to track real-time demand, automatically identifying gaps in coverage based on patient acuity, census data, and staff availability. Managers can post open shifts to the float pool, allowing qualified team members to claim them based on their credentials and preferences—or the system can auto-assign shifts using predefined rules to ensure fairness.
The software also helps maintain balance by tracking hours worked, certifications, and unit-specific competencies, preventing burnout by capping shifts or rotating assignments equitably. Alerts notify schedulers when high-priority areas need immediate support, reducing reliance on manual oversight.
Why Do Hospitals Use Internal Float Pools?
Hospitals use float pools for a variety of reasons, particularly retention of late career staff, offering flexible or part time work, preserving known career locums physicians that return to the system over and over again, and as a way to attract and engage physicians that you may not yet have a full-time position for. Overall, float pools are a great recruitment and retention tool! Here’s why:
Offer Flexible Schedules for Providers
Many physicians and advanced practice providers (especially those approaching retirement or who face unexpected live events) aren’t looking to stop working entirely. Instead, they want flexibility. Float pools allow hospitals to offer reduced hours or part-time assignments, non-continuous shifts (e.g., one week per month), and local-only or low-travel options. This helps retain experienced clinicians who still want to contribute but no longer want the demands of full-time work.
Create a “Bridge to Retirement” Pathway
Hospitals can formalize float pool participation as a step-down option for employed providers. This gives clinicians more control over their exit timeline while keeping coverage internal — avoiding more expensive external locum options.
Retiring or semi-retired providers often have deep relationships with patients, staff, and the community. Keeping them in the system through float work:
- Preserves institutional knowledge
- Smooths transitions
- Enables mentorship of younger clinicians
- Reduces disruption in care continuity
Recapture Underutilized Availability
For providers who have shifted away from full-time practice (e.g., leadership roles, academic positions, or phased retirement), float pools give the hospital a way to tap into their remaining clinical availability and fill short-term gaps without full reactivation.
Boost Retention by Providing Variety
Some mid-to-late career clinicians seek variety instead of volume. Working across multiple departments, locations, or shift types through the float pool can re-engage providers, delay burnout, and keep them in the system longer.
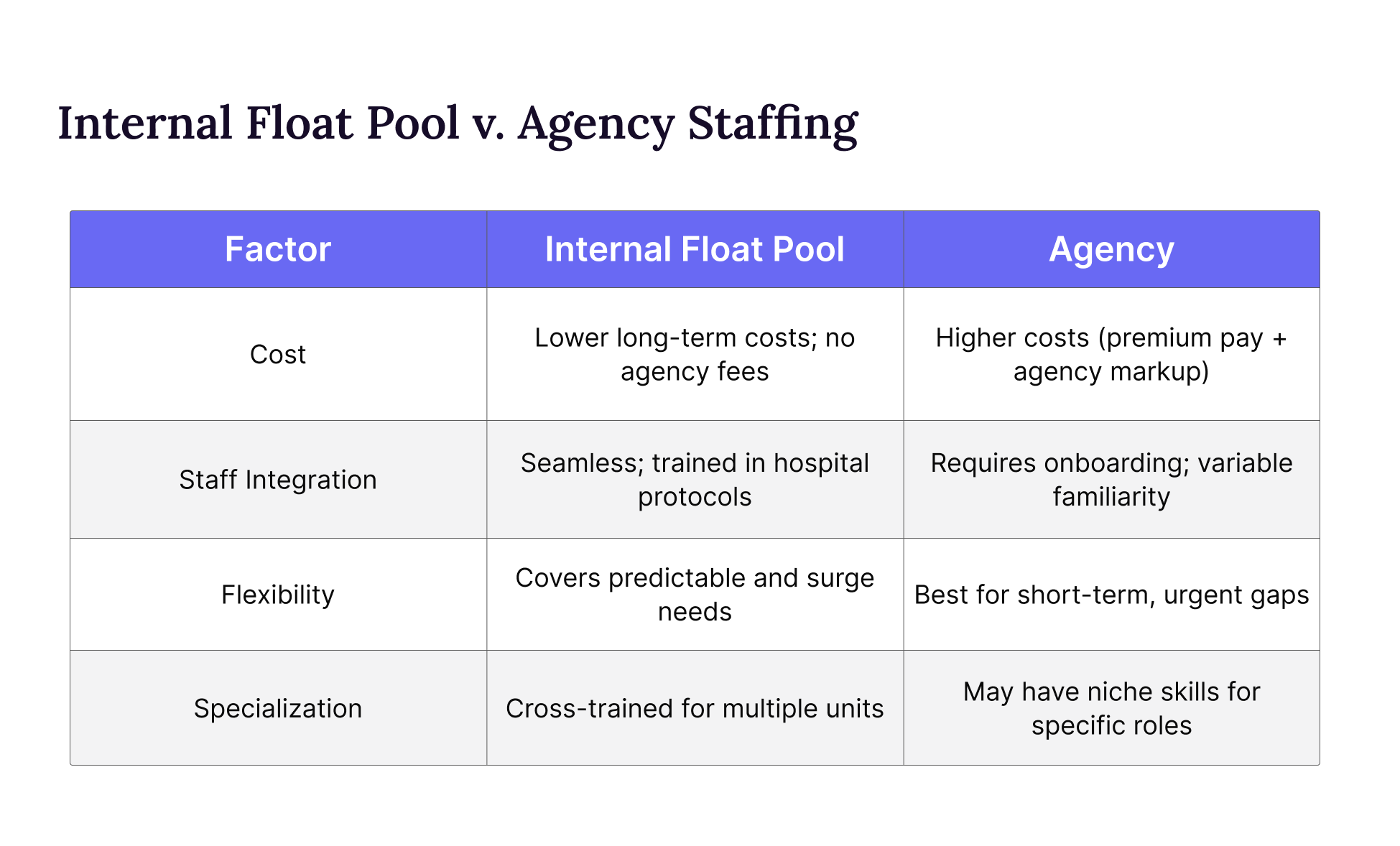
What’s the Difference Between Using a Float Pool and an Agency?
While both float pools and agency staffing provide hospitals with flexible workforce solutions, they operate in fundamentally different ways. A float pool consists of known clinical support staff that a hospital can tap as demand fluctuates. It creates a resource of providers who have more familiarity with the facility’s protocols, systems, and culture. These professionals move between departments as needed but remain integrated into the organization.
Agency staff, on the other hand, are external contractors hired through third-party firms. While they offer quick fixes for sudden shortages, they often come at a higher cost and may require additional onboarding to align with hospital-specific procedures. Because agency workers are not permanent employees, they may lack the same level of institutional knowledge or long-term commitment.
Ultimately, float pools provide consistency and cost efficiency, while agency staffing serves as a short-term contingency. Hospitals that invest in strong float pools often see better care continuity, smoother operations, and greater financial sustainability.
How Does Float Pool Scheduling Work?
Float pool scheduling for physicians and APPs (sometimes called internal locums, an internal agency, or simply a provider float pool) gives hospitals flexible access to credentialed clinicians already familiar with their system. It’s a powerful way to reduce external staffing costs, fill last-minute needs, and improve continuity of care. But unlike nursing float pools, managing physician float pools requires more complexity around credentialing, compensation, communication, and coverage governance.
Visibility and Centralized Coordination
It starts with identifying everyone in the system who’s already working shift-based or part-time: moonlighters, PRNs, semi-retired providers, or full-time clinicians with availability. Then, centralize those opportunities and availability in one place—often through a VMS or internal scheduling tool—to match open shifts with the right clinicians.
Defined Ownership and Accountability
For a float pool to function, someone has to own it. That means:
- Knowing who pays the provider
- Managing credentialing and malpractice
- Coordinating scheduling and communication
- Ensuring alignment across departments and facilities
Flexible Yet Governed Scheduling
Providers may self-schedule, be offered predictive assignments, or respond to short-notice requests. Some float pools offer a base shift guarantee with optional pickup; others run entirely on-demand. Either way, there must be a system that balances provider preferences with hospital needs.
Skill-Based Matching
Not every provider can work every shift. Advanced float pool programs use workforce systems to match clinicians based on specialty, privileges, facility familiarity, and even shift type, ensuring providers are appropriately deployed and quality of care is protected.
Mechanism to Grow the Pool
Beyond internal moonlighters, hospitals can—and should—proactively grow their float pool. High-value sources include:
- Transitioning Retirees – Offering flexible schedules to experienced clinicians who want to phase out of full-time work.
- Travel Clinicians Open to Local Assignments – Engaging travel nurses or locum tenens providers who prefer local opportunities.
- Cross-Training Existing Staff – Expanding the pool by training current employees in adjacent specialties or units.
- Partnerships with Staffing Agencies – Collaborating with trusted vendors to supplement the float pool during demand surges.
How to Optimize Cost and Coverage with a Physician Float Pool
A well-managed physician and advanced practice float pool is one of the most powerful tools a health system can use to control labor costs, reduce agency dependency, and ensure consistent patient coverage. But float pools don’t manage themselves, and simply having a list of moonlighters isn’t enough.
To realize real ROI, organizations need a deliberate strategy: one that tracks historical demand, builds internal capacity in high-utilization specialties, and uses technology to align provider availability with system-wide needs. With the right structure in place, float pools can shift staffing from reactive to proactive—driving cost savings, increasing provider engagement, and protecting continuity of care.
Analyze Historical Data to Anticipate Demand
Use past trends to forecast seasonal surges, provider absences, and onboarding delays—so you can proactively schedule float pool coverage instead of paying last-minute agency rates.
Implement a Tiered Float Pool Strategy
Categorize float pool members by specialty, cost, and flexibility to ensure you’re deploying providers appropriately. Not every shift requires a high-cost specialist.
Determine Where You Consistently Rely on Locum Coverage
These are the first specialties to target for internal float pool recruitment. Over time, this reduces your external spend and gives you more control.
Don’t Overlook Low-Volume Specialties
Just because you only need oncology or cardiology coverage a few months a year doesn’t mean those providers shouldn’t be in your float pool. Proactively recruit, credential, and schedule them in advance—so they’re ready when the need returns.
Maximize Internal Resources Before Outsourcing
Before opening a shift to external agencies, ensure you’ve exhausted internal capacity. With the right technology, you can quickly identify who’s available across your system and fill more shifts in-house.
Other FAQs about Float Pools
Do Float Pool Providers Get Paid More?
Often, yes—but the overall cost to the hospital may still be comparable to full-time employees. Float pool physicians and advanced practice providers typically receive higher hourly or per-shift pay due to their flexibility, short-notice availability, and willingness to work nights, weekends, or holidays.
However, float pool providers are often not eligible for benefits like health insurance, retirement contributions, or paid time off. As a result, while their base rate may be higher, the total cost of employment can be similar—or even lower—than that of a full-time, benefited employee.
For providers, the trade-off is clear: they gain more autonomy and often higher pay per shift, but forego traditional benefits. For hospitals, float pools offer a way to meet demand flexibly without long-term employment overhead.
What Are the Pros and Cons of Float Pool Work?
Float pool shifts offer unique advantages, including higher pay rates, diverse clinical experiences, and the opportunity to sharpen adaptability across multiple units. Providers often enjoy varied schedules and reduced monotony, along with the chance to build relationships hospital-wide. For hospitals, float pools provide staffing flexibility and cost savings compared to agency reliance.
However, the role comes with challenges. The most common concern providers express around float pools is inconsistency. While some individuals thrive in such a role, others miss the stability of a fixed unit and schedule. Unit-specific protocols or unfamiliar equipment may require quick learning curves, and some providers find it harder to establish deep roots through float pool work.
How Does Syncx Float Pool Work?
At Syncx, we don’t just manage your float pool—we become an extension of your team, fully invested in your success. Our unique partnership model means we’re incentivized as your float pool grows and you save money, creating a shared commitment to long-term results.
We specialize in helping facilities staff physicians, advanced practice providers, and CRNAs where they’re most needed. Our experts assist you with every detail, from recruiting top-tier talent and streamlining credentialing to managing payroll and deploying cutting-edge technology. We bring years of proven experience in building high-performance float pools, ensuring your program is scalable, sustainable, and resilient no matter the circumstances.
With Syncx, you’re gaining more than a service provider. You’re gaining a strategic partner dedicated to optimizing your workforce, reducing costs, and maintaining seamless patient care with fully custom, tech-forward solutions. Ready to transform your float pool into a competitive advantage? Let’s talk.

