The quiet crisis haunting healthcare isn’t just a shortage of staff—it’s a failure to keep them. Hospitals and health systems across the country are in a relentless cycle of recruiting, hiring, and training, only to watch valuable employees walk away, often within their first year. The cost is staggering, measured not only in financial terms but in lost institutional knowledge, team morale, and the quality of patient care.
The root causes are well-known: culture shock for new hires, unsustainable workloads, and a lack of support that leads to burnout. But within this challenge lies a profound opportunity. What if the key to solving the staffing crisis isn’t just finding more people, but creating an environment where your current talent chooses to stay and build their careers? This article outlines ten actionable retention strategies that go beyond quick fixes, offering a blueprint for healthcare leaders ready to foster a resilient, engaged, and loyal workforce where both people and patients can thrive.
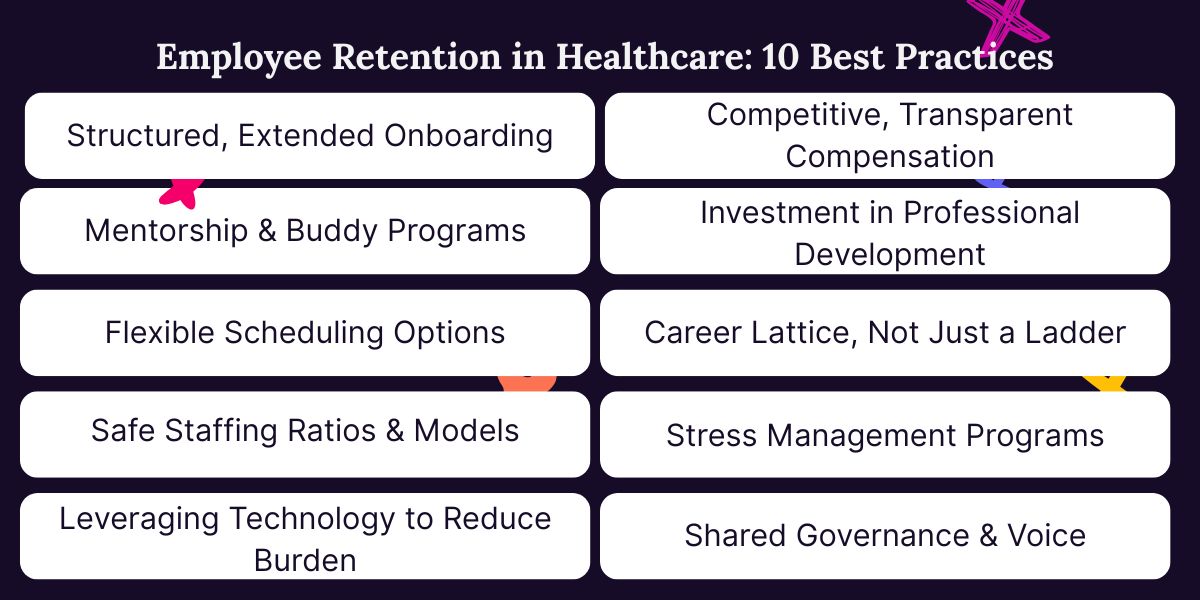
1. Structured, Extended Onboarding
The first few months at a new healthcare organization are a critical period that can determine an employee’s entire tenure. Too often, onboarding is a rushed process involving a whirlwind of HR paperwork, IT logins, and an all-too-brief tour of the facility. This approach leaves new hires feeling unprepared and disconnected, exacerbating the culture shock that is one of the driving factors behind early exits. To truly retain talent, healthcare organizations must start to view onboarding as a strategic, extended process of integration that lasts for at least the first 90 days.
An effective extended onboarding program is a deliberate journey designed to acclimate new staff both clinically and culturally. Some successful programs include support for up to the first two years of a new hire’s role. Such programs can include not only frequent meetings with managers but also intentional introductions to key team members across different departments, fostering a sense of belonging and clarifying how their role fits into the larger patient care ecosystem. By slowing down the process and providing sustained support, organizations demonstrate a genuine investment in their new employee’s success, transforming a period of potential anxiety into one of confident integration.
2. Mentorship & Buddy Programs
While a structured onboarding program provides the framework for success, a mentorship or buddy program provides the human connection that brings it to life. Being the “new person” in a fast-paced healthcare environment can be isolating; having a designated go-to person can make all the difference. A buddy system pairs a new hire with an experienced, well-respected peer who acts as a friendly guide, a safe source for questions, and a cultural translator. This relationship alleviates the immense pressure new employees feel to have all the answers immediately, reducing the stress that leads to burnout and turnover.
The power of an effective mentorship program lies in its informality and peer-to-peer dynamic. A mentor is not a supervisor; they are a confidant who can explain the unwritten rules of the unit, share shortcuts, and offer encouragement after a tough day. This support system helps new staff navigate not just clinical procedures, but also the complex social and emotional landscape of the workplace. This simple yet profound strategy ensures that new employees feel seen, supported, and valued from day one, building the strong interpersonal bonds that are essential for long-term retention.
3. Flexible Scheduling Options
The traditional, rigid schedule of healthcare is a primary driver of burnout, pushing seasoned professionals toward early retirement and overwhelming those seeking a better work-life balance. To retain this critical institutional knowledge and adapt to modern workforce demands, organizations must rethink flexibility not as a perk, but as a strategic imperative. One powerful solution is the creation of robust internal float pools. These pools offer a sanctioned pathway for experienced staff to step away from the demands of a full-time schedule without severing their ties to the organization.
For a veteran doctor or nurse nearing retirement, the float pool model provides a graceful transition, allowing them to contribute their invaluable expertise on a limited basis, mentoring newer staff while enjoying a more manageable pace. Simultaneously, for staff experiencing burnout, the float pool offers a vital pressure valve by providing an opportunity to reduce hours, explore different units, or take extended time off without having to resign. By formalizing these flexible options, healthcare organizations demonstrate a commitment to meeting employees at their current life stage, transforming a potential exit into a sustainable, long-term relationship that benefits both the individual and the institution.

4. Safe Staffing Ratios & Models
The pursuit of safe staffing is a constant battle against patient acuity fluctuations, unexpected leave, and recruitment gaps. Even with the best intentions, internal efforts to maintain safe ratios can be overwhelmed, leading to mandatory overtime and burnout among permanent staff. This is where a strategic partnership with a managed service provider (MSP) for locum tenens becomes a critical component of a sustainable staffing model.
An MSP acts as an extension of your team, providing a reliable, vetted pipeline of qualified temporary providers to fill scheduled vacancies and unexpected shortages swiftly. This proactive support prevents your core staff from being stretched to a breaking point. By seamlessly integrating locum tenens coverage through a trusted partner, organizations can finally move from reactive crisis management to proactive stability. This approach demonstrates a tangible commitment to safe staffing, protecting both patient safety and the well-being of your permanent team, which is the ultimate foundation of retention.
5. Leveraging Technology to Reduce Burden
In the demanding environment of healthcare, administrative tasks often feel like a second, unpaid job that pulls clinicians away from their primary mission. The burden of manual charting, tracking down equipment, and navigating clunky communication systems contributes significantly to daily frustration and burnout. To retain modern healthcare talent, organizations must adopt tools that simplify workflows, automate mundane tasks, and free up valuable cognitive space for clinical decision-making and human connection.
This is where specialized software, particularly in areas like managing locum tenens staff, proves its value. Instead of relying on a labyrinth of spreadsheets, emails, and phone calls to coordinate temporary providers, a unified platform can streamline the entire process from credentialing and scheduling to communication and payment. This efficiency doesn’t just benefit the administrators; it directly reduces the burden on permanent staff. When a locum tenens provider can be seamlessly integrated into the team with all necessary information at their fingertips, it prevents disruptions and ensures the entire unit functions smoothly.
6. Competitive, Transparent Compensation
While passion for patient care is the driving force for many in healthcare, fair compensation remains the essential foundation of any successful retention strategy. In a competitive labor market, failing to offer salaries and benefits that reflect the immense skill, responsibility, and dedication of healthcare workers is a direct invitation for them to seek opportunities elsewhere. However, this strategy is only made truly effective by pairing competitive pay with a culture of transparency. When employees understand how their compensation is determined and see evidence that it is fair and equitable, it builds a crucial layer of trust between them and the organization.
Transparency in compensation means having clear, well-communicated salary structures based on objective criteria like experience, specialties, and credentials. It involves conducting regular market analyses to ensure pay scales remain competitive and adjusting them accordingly. This approach eliminates the suspicion and frustration that fester when pay feels arbitrary or secretive, which is often a silent driver of turnover.
7. Investment in Professional Development
For dedicated healthcare workers, the opportunity to grow their skills is a core component of professional fulfillment. An organization that actively invests in the professional development of its staff sends a powerful message of support. This investment can take many forms, from providing tuition reimbursement for advanced degrees to offering subsidies for specialized certifications or attendance at key industry conferences. It also includes hosting regular in-service training on new equipment, procedures, or evidence-based practices.
By creating clear pathways and providing resources for continuous learning, the organization positions itself as a partner in the employee’s career journey, not just a place of employment. When staff see that their employer is willing to invest in sharpening their skills and expanding their knowledge, they are far more likely to envision a future within that organization.
8. Career Lattice, Not Just a Ladder
The traditional career path often resembles a narrow ladder, with the only visible route for advancement leading away from patient care and into management. This model forces a difficult choice upon exceptional clinicians: remain in the clinical role they love but face limited growth, or sacrifice their passion for hands-on care to move “up.” This false dichotomy is a significant source of talent drain. To retain top performers, forward-thinking organizations are replacing the ladder with a lattice, a framework that supports multidirectional growth.
A career lattice acknowledges that growth is not one-dimensional. It creates formal programs that allow frontline staff to advance in title, responsibility, and compensation by becoming clinical experts, unit-based educators, or quality improvement specialists. It encourages and facilitates lateral moves into different specialties, allowing an employee to explore new areas of interest without leaving the organization.
9. Stress Management Programs
The high-stakes, emotionally charged nature of healthcare makes stress an inherent part of the job. However, when chronic stress is left unaddressed, it evolves into burnout, compassion fatigue, and ultimately, turnover. While individuals can practice personal coping techniques, studies show that organizational support for stress management provides a range of benefits, including employee retention.
Effective programs are multi-faceted and integrated into the fabric of the organization. This includes providing subscriptions to meditation and mindfulness apps, offering on-site yoga or resilience training workshops, and, most importantly, normalizing the use of counseling. Leadership can further reinforce this commitment by creating dedicated “quiet rooms”—spaces for brief respite during a shift—and, crucially, by actively encouraging staff to take their breaks and use their paid time off without guilt. When an organization invests in these resources, it helps to de-stigmatize the discussion around mental health and provides a vital safety net, empowering staff to manage the immense pressures of their roles sustainably.
10. Shared Governance & Voice
For healthcare professionals who make critical decisions every day, feeling powerless over the conditions of their own work is a profound source of frustration and disengagement. A top-down approach where policies and procedures are dictated without frontline input ignores the most valuable source of insight: the people doing the work. Shared governance is a structural model that flattens this hierarchy, giving nurses and other clinical staff a formal voice and authentic decision-making authority in matters that affect their practice, their environment, and ultimately, patient care.
This model establishes unit-based councils or committees where frontline staff can review data, propose solutions, and lead initiatives related to clinical practice, quality improvement, and professional development. Whether it’s involving them in selecting new patient-lift equipment, redesigning a workflow for efficiency, or contributing to scheduling policies, shared governance fosters a sense of ownership and professional respect.
Ready to Build a Workplace Where Talent Stays?
The journey to better retention starts with empowering your people and streamlining your processes. Syncx was built specifically for healthcare organizations that understand this connection. Our locum tenens software and internal float pool solutions reduce the administrative friction that burdens your permanent staff, simplifies scheduling to support work-life balance, and ensures every provider is seamlessly integrated into your team.
Stop letting operational inefficiencies drive your best people away. Schedule a free Syncx demo and see how the right technology can be your most powerful retention tool.
