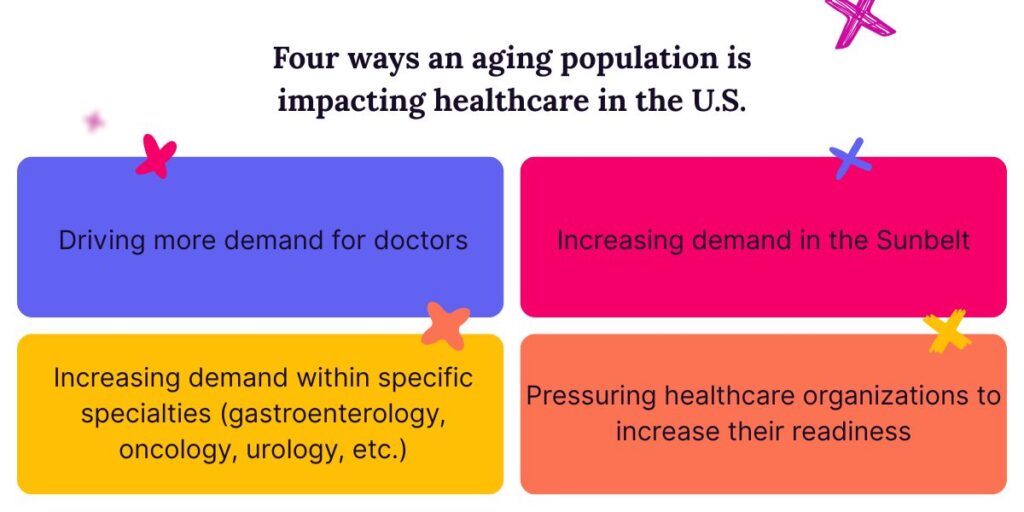
The aging of today’s older generations is fundamentally reshaping how healthcare is delivered. By 2030, about one in five people in the United States will be at the age of retirement. An aging population presents two primary challenges to any healthcare system: a soaring demand for complex, specialized care and an intensifying competition for the clinical talent required to provide it.
This article is designed to equip you with the insights to navigate this new reality. We will examine how aging populations are driving acute staffing shortages, creating geographic hotspots of demand, and elevating specific specialties to critical importance. Most importantly, we will explore the proactive solutions that can help your organization not just respond, but build a sustainable and resilient workforce for the future. Let’s get started.
Aging Populations Are Driving a Healthcare Staffing Shortage
As the Baby Boomer generation ages, a larger percentage of the population now requires more frequent and complex medical care, from managing chronic conditions to post-acute rehabilitation. This surge in demand directly collides with a parallel reality: a significant segment of the current clinical workforce is approaching retirement age itself. This dual pressure—more patients requiring care and fewer experienced providers available to deliver it—creates a perfect storm, straining hospitals, clinics, and long-term care facilities.
In addition to providing stronger retention and recruitment programs, optimizing the existing workforce through advanced technology and revised care models can help maximize the impact of every clinician. For example, many hospital organizations are increasingly utilizing an “internal float pool” in order to retain physicians who are near retirement by offering them more flexible work options.
Aging Populations Drive Demand in Specific Parts of the Country
While the aging trend is national, its impact on healthcare demand is profoundly localized, creating acute staffing challenges in specific regions. Popular retirement destinations across the Sun Belt—such as Florida, Arizona, and parts of Texas—are experiencing population growth rates among seniors that far outpace the national average.
For healthcare executives, understanding these specific migration and demographic patterns is essential. Strategic staffing must involve analyzing regional population forecasts, competitor density, and local educational capacity to build proactive talent pipelines. An MSP partner with national reach and local market intelligence becomes invaluable in this scenario, capable of deploying resources strategically, sourcing candidates from wider networks, and implementing compensation and incentive models calibrated to these high-demand markets.

Specific Specialties Are on the Rise Due to an Aging Population
As the population ages, it creates intense competition for professionals in geriatrics, cardiology, orthopedics, oncology, and palliative care. These specialties are critical to managing the chronic and complex conditions prevalent among older adults. And while the U.S. might need more than 30,000 geriatric specialists to meet the needs of its aging population, only 7,500 were employed in 2023.
To meet this specialized demand, organizations must proactively build and sustain these talent pipelines. This requires partnerships with medical and nursing schools to influence curriculum and foster interest in geriatric-focused care, as well as investing in robust residency and fellowship programs. Equally important is creating clear clinical ladders and continuing education pathways that allow existing staff to subspecialize, transforming generalist nurses into certified geriatric care managers, for example.
A partnership with a Managed Service Provider (MSP) can be instrumental in this effort, leveraging market intelligence to identify sourcing channels for these high-demand specialties and helping to design competitive compensation packages that attract and retain this elite clinical talent.
Organizations May Not Be Ready to Meet the Needs of a Large Aging Population
Despite the clear demographic trends, a significant readiness gap threatens many healthcare organizations. Many institutions are still operating with legacy care models and workforce strategies designed for a younger patient mix, lacking the infrastructure, training, and cultural competencies essential for geriatric care. This gap manifests in physical spaces not designed for mobility challenges, EHR systems not optimized for managing multiple chronic conditions, and clinical workflows that fail to account for the increased social complexities that emerge when treating older adults.
Closing this readiness gap demands a top-down commitment to age-friendly health systems. Leadership must champion initiatives that embed geriatric best practices into the fabric of the organization, from adopting the “4Ms” framework (What Matters, Medication, Mentation, Mobility) to redesigning physical environments for safety and accessibility.
Proactive Healthcare Staffing Solutions
The challenge of matching specialized talent with specific regional demands is complex, but you don’t have to tackle it alone. At Syncx, we combine deep healthcare expertise with intelligent workforce technology to deliver tailored MSP solutions. Our data-driven approach helps you anticipate staffing needs, secure in-demand specialties, and implement flexible retention strategies that transform your workforce from a cost center into a competitive advantage.
Ready to move from reactive staffing to proactive workforce strategy? See firsthand how Syncx can help you build a sustainable talent pipeline and optimize your operations to meet the needs of an aging population.
Schedule a personalized demo today and let us show you how our platform and expertise can help you prepare, adapt, and lead in the evolving healthcare landscape.
