Imagine this: one of your best doctors, a dedicated professional who always goes the extra mile, suddenly turns in her resignation. And it isn’t because she found a better salary elsewhere. Rather, she’s suffering under the relentless strain of being constantly short-staffed and the moral distress of feeling unable to provide the care she knows her patients deserve. This scenario is a daily reality in healthcare facilities across the country, and it’s costing organizations dearly in turnover, burnout, and compromised patient safety.
While the passion to heal is what draws people to healthcare, systemic pressures are what too often drive them away. Understanding and improving the well-being of your workforce is a critical strategic imperative directly tied to your organization’s financial health and quality of care.
But you can’t fix what you don’t measure. This guide provides actionable strategies for gaining genuine insights into workforce satisfaction. We’ll explore how to listen effectively, interpret the signals, and, most importantly, how to take action. It all begins with addressing the most fundamental stressor: ensuring your team has the stable, supportive staffing foundation they need to thrive.
Why Is Working in Healthcare so Stressful?
Healthcare professionals are driven by a profound commitment to healing and helping others. Yet, the very environment designed for care can often be a crucible of stress. Understanding these pressures is the first step toward alleviating them. The challenges are multifaceted, but they often stem from a few core issues:
High-Stakes Responsibilities
There is no room for error. Physicians, nurses, and allied health professionals make decisions that directly impact human lives daily. This immense responsibility creates a persistent, underlying pressure that is unlike almost any other field.
Emotional Toll and Compassion Fatigue
Healthcare workers are on the front lines of human suffering, grief, and trauma. Continuously supporting patients and families through critical times, often while managing their own emotional responses, can lead to compassion fatigue and emotional exhaustion.
Administrative Burden and Documentation
The increasing demand for electronic health record (EHR) documentation, compliance reporting, and administrative tasks pulls time away from direct patient care. This “charting at home” phenomenon contributes significantly to frustration and work-life imbalance.
The Domino Effect of Staffing Gaps
This is a primary and pervasive stressor. When a team is understaffed due to factors like vacancy, illness, or leave, the ripple effects are immediate and severe. Remaining staff face:
- Increased Patient Loads: Safely managing more patients than is optimal.
- Mandatory Overtime: Disrupting personal lives and leading to burnout.
- Moral Distress: The painful feeling of being unable to provide the standard of care they know patients deserve due to systemic constraints like being short-staffed.
This constant cycle of being overworked and under-resourced is a direct pipeline to burnout, making the role of a healer increasingly unsustainable.
Why Measuring Satisfaction Is More Critical than Ever
Staff satisfaction isn’t a soft metric; it’s a hard indicator of care quality. Numerous studies confirm that burned-out, dissatisfied clinicians are more prone to medical errors. Conversely, a supported, engaged workforce leads to higher patient satisfaction scores (HCAHPS), better adherence to safety protocols, and improved overall patient outcomes. Investing in your staff’s well-being is directly investing in patient safety.
Furthermore, the financial drain of constant staff turnover is staggering. Consider the costs of recruiting, signing bonuses, onboarding, and training new hires, not to mention the lost productivity during vacancies. Measuring satisfaction allows you to identify and address problems before they lead to an exit, protecting your organization’s bottom line. It is far more cost-effective to retain a current employee than to recruit a new one.
Satisfaction data provides concrete evidence of what’s working and what isn’t, allowing leadership to pinpoint specific friction points. Ultimately, measuring workforce satisfaction provides the crucial insights needed to build a resilient, stable, and high-performing organization.
How to Measure Staff Satisfaction in Healthcare?
Understanding the “why” behind measurement is only the beginning. The next step is implementing effective methods to gather genuine, actionable feedback. The goal is to move beyond guesswork and create a clear, data-driven picture of your team’s experience. This requires a multi-faceted approach that values both anonymity and direct conversation.
The Anonymous Survey (The Gold Standard)
The anonymous survey remains one of the most powerful tools in your arsenal. Its primary strength is its ability to elicit candid feedback that staff might be hesitant to share openly for fear of repercussion.
To be effective, these surveys must be carefully constructed. A blend of quantitative and qualitative questions works best. Using validated, industry-standard tools like the Mini-Z Survey for physician burnout provides crucial insights that can directly translate to tangible change. The key to a successful survey initiative is transparency; you must communicate the results back to the staff and, most importantly, outline the actionable steps you will take in response. This builds trust and shows that their voices have been heard, making them more likely to participate in the future.
The Power of Stay and Exit Interviews
While surveys provide broad data, interviews offer deep, personal context. Proactive “Stay Interviews” are an invaluable yet underutilized strategy. These involve having leaders or HR sit down with high-performing, tenured employees to ask a simple but profound question: “What motivates you to stay here, and what could we do to make your experience even better?” The answers provide a roadmap to your organization’s strengths and opportunities for improvement directly from your most valuable players.
Conversely, “Exit Interviews” conducted with departing employees are a critical learning opportunity. When handled with empathy and a genuine desire to learn, they can uncover systemic issues that may not surface in surveys. The goal is not to convince the employee to stay but to understand the root causes of their departure.
Focus Groups and Listening Sessions
While surveys provide the “what,” focus groups and listening sessions help you understand the “why.” These facilitated conversations, led by a neutral party from HR or an external moderator, create a safe space for staff to discuss their experiences in depth.
The key to success is asking open-ended questions that encourage dialogue rather than simple answers. Inquire about daily workflow hurdles, the quality of communication between teams, or ideas for improving support. This approach signals to your staff that leadership is not just checking a box but is genuinely invested in listening to their lived experiences and valuing their collective expertise in problem-solving.
Indirect Metrics: Reading the Tea Leaves
Often, the signs of workforce dissatisfaction are visible long before an official survey is ever conducted. Astute healthcare leaders learn to recognize these indirect metrics like high rates of absenteeism, especially unplanned absences on Mondays or Fridays, which can be a telltale sign of disengagement and burnout. Similarly, a creeping reliance on mandatory overtime or a sudden spike in the use of sick time often points to an overwhelmed workforce.
Beyond scheduling data, other operational metrics can serve as powerful proxies for satisfaction. Employee turnover rate remains the most stark indicator, but even patient feedback can offer clues. A rise in patient complaints about wait times, communication, or perceived staff hurriedness may not reflect a lack of care but rather a team stretched too thin to provide the level of care they aspire to.
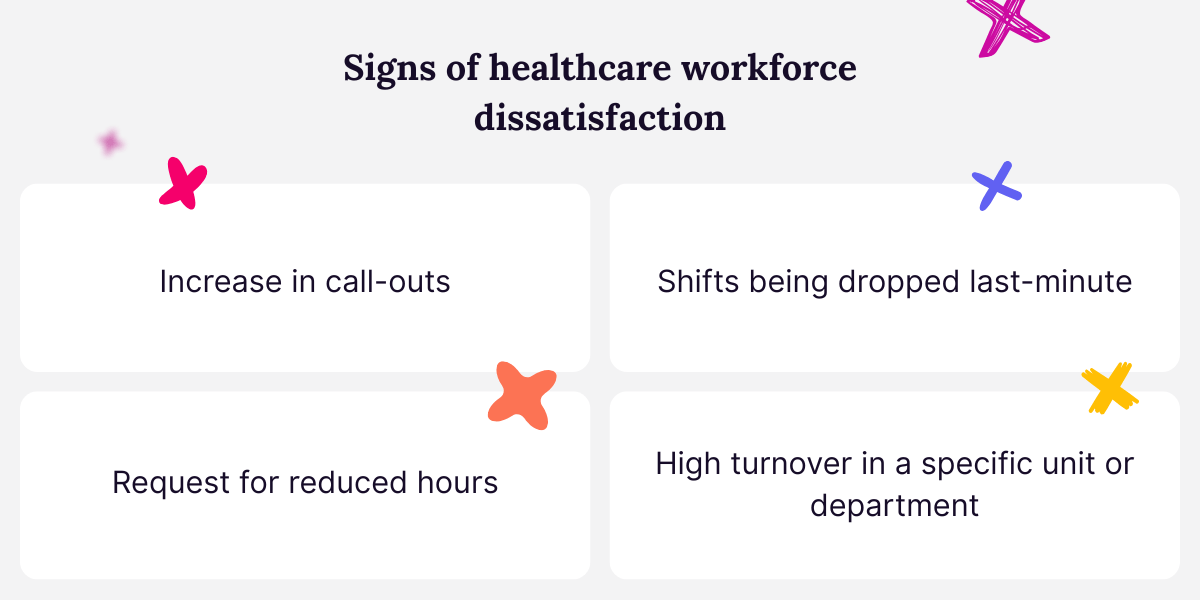
Signs of Dissatisfaction in the Healthcare Workforce
While surveys and interviews provide direct insight, often the earliest warnings of workforce dissatisfaction manifest in day-to-day operations, especially through chronic staffing gaps. These gaps are both a cause and a symptom of discontent, creating a cycle that can be difficult to break.
Learning to recognize these signs is crucial for proactive intervention. Look for patterns like a sudden increase in last-minute call-outs, which can signal that employees are feeling overwhelmed and need relief. Similarly, a rise in requests for reduced hours or shifts being dropped at the last minute often points to a team stretched to its limit, struggling to maintain work-life balance. Strategic resources like Syncx MSP are vital for not only identifying patterns in staffing gaps but also filling them proactively.
Perhaps most telling is an increase in turnover within a specific unit or role; when skilled, experienced professionals start leaving, it’s a clear indicator that underlying issues (such as unsustainable workloads, moral distress, or a lack of support) have gone unaddressed. These patterns rarely exist in isolation. Over time, what begins as a manageable challenge can spiral into a crisis, eroding trust in leadership and undermining the stability of the entire team.
Turning Healthcare Workforce Satisfaction Data into Action
Satisfaction data’s true value is realized only when translated into meaningful action. The first step is to close the feedback loop by communicating the findings transparently with your staff. Sharing a summary of what you learned demonstrates that their voices were heard and validates their experiences.
Next, prioritize the issues raised and create a concrete action plan with clear ownership and timelines. This plan must address both quick wins and larger, systemic initiatives. Perhaps survey results reveal frustration with administrative burdens, leading to a pilot program for streamlined documentation. Maybe focus groups highlight inconsistent communication, sparking the implementation of daily leadership huddles.
The crucial element is to start, to show tangible progress, and to re-measure periodically. This creates a virtuous cycle of feedback and improvement, building trust and proving that the organization is committed to fostering a better environment.
Reduce Burnout by Solving Staffing Gaps
Ultimately, the most pervasive catalyst for burnout—and the most critical issue your satisfaction data is likely to uncover—is chronic understaffing. You can host all the listening sessions you want, but if your clinicians are consistently facing excessive patient loads and mandatory overtime, satisfaction will remain elusive.
The most effective action you can take is to build a resilient staffing strategy that proactively prevents these gaps from occurring. This means moving beyond reactive crisis management and creating a seamless, reliable pipeline of qualified temporary professionals who can integrate quickly and maintain continuity of care during vacancies, leaves, or periods of high demand.
Ready to build a more stable foundation for your team and protect your permanent staff from burnout? See how Syncx provides a seamless, reliable solution for managing your locum tenens staffing needs. Request a demo today to discover how you can ensure continuity of care and create a more sustainable work environment.
